Contents
1. The wider maltreatment context around ACEs
‘Ten Adverse Childhood Experiences – ‘The ‘Classic ACEs Profile’
3. Current definition of ACEs
4. The cycle of ACEs
1. Measuring ACEs
2. The pathways to adult mental and physical ill-health
3. The prevalence of ACEs
4. Intervention to modify and prevent the impact of ACEs
1. Toxic Stress and Trauma-Informed Care
2. ACEs Trauma-informed practice
3. The effects of reducing ACEs – Health Equity
4. A systematic review of trials to improve child outcomes associated with ACEs
5. Parallel developments: The Framework for the Assessment of Children in Need and their Families (2000)
6. The Hope for Children and Families Modular Programme
1. A Pair of ACEs
2. Relationship between ACEs and deprivation
3. The Covid-19 pandemic as an Adverse Experience
4.The impact of climate change on mental health and emotional well-being
5. Exposure to harmful influences online
6. The Hope for Children and Families Modular Programme
1. Direct research with children and young people
2. Forty forms of Adverse Experiences
3. A National Traumatic Stress Survey
4. The harmful effects of ACEs associated with children and young people in conflict with the law
5. Suicidal ideation and adversity
6. Traumatic experiences of foster care and children and young people
7. The impact of neglect
8. Spanking and adult mental health impairment: The case for the designation of spanking as an Adverse Childhood Experience
1. Lifespan outcomes of Adverse Childhood Experiences and costs to the community
2. Outcomes associated with ACEs
3. Costs associated with ACEs
4. Factors which protect against the impact of ACEs
5. Strengths and limitations of the ACEs score
6. The ACEs score does not predict poor health outcomes at the individual level
7. Research on risk calculators to identify which children exposed to ACEs will develop poor health outcomes
8. Adverse Childhood Experiences are associated with neurobiological and inflammatory responses
1. The wider maltreatment context around ACEs
Maltreatment has been increasingly recognised over past decades including the emergence of different types of child abuse.
A recent review outlines the historical, social and research contexts in which ACEs emerged from the extensive maltreatment literature. The current political and financial implications for practice and research are discussed (Vizard, Gray & Bentovim, 2021, p.1, p.9)
Definition of ACEs in Felitti et al.’s 1998 study
Vincent Felliti and his colleagues at the Kaiser Permanente Organisation (1998) defined Adverse Childhood Experiences as follows:
2. ‘Ten Adverse Childhood Experiences – ‘The ‘Classic ACEs Profile’
- Physical neglect: failure to supervise or provide for the child
- Emotional neglect: caregiver unable to express affection or love for the child due to personal problems
- Physical abuse: severe assault or physical abuse such as shaking or hitting
- Sexual abuse: child experienced sexual abuse or forced sex
- Emotional abuse: caregiver engaged in psychological aggression towards the child such as threatening
- Caregiver treated violently: domestic violence of an adult in the home including slapping hitting or kicking
- Caregiver substance-abuse: active alcohol and drug abuse by a caregiver
- Caregiver mental illness: serious mental illness or elevated mental health symptoms
- Caregiver divorce/family separation: child’s parent(s) deceased, separated or divorced or child was abandoned or placed in out of home care
- Caregiver incarceration: caregiver spent time in prison or is currently in jail or detention centre
What was unique in Fellitti et al.’s approach was that they established an “ACE score” by summing the number of ACEs reported by more than 17000 adults in the USA. The study showed that the higher the ACE score, the stronger the association was with poor subsequent health as adults, and the greater their risks of health-harming behaviours heart disease, cancer, stroke, type 2 diabetes, chronic bronchitis, fractures, hepatitis and poor self-rated health.
3. Current definition of ACEs
ACEs are defined as experiences which require significant adaptation by the developing child in terms of psychological, social and neurodevelopmental systems, and which are outside of the normal expected environment (adapted from (McLaughlin, 2016). ACEs may include other adversities not included in Felitti et al.’s 1998 study, such as bullying victimisation, parental death, and community violence.
4. The cycle of ACEs
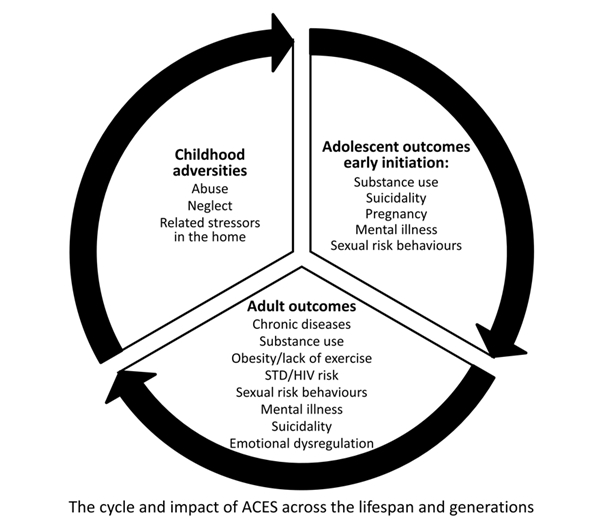
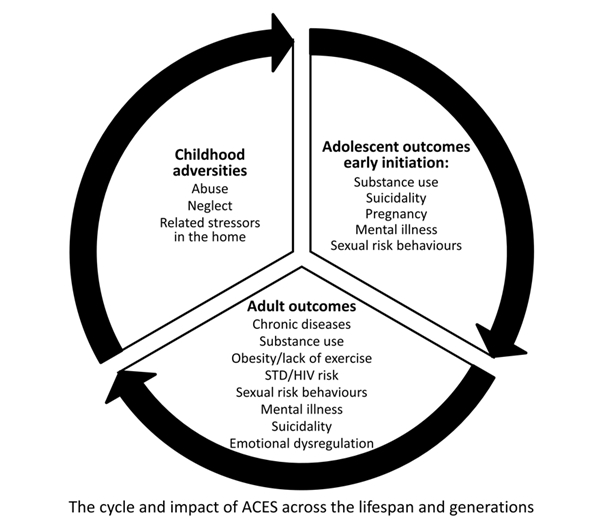
Shanta Dube recently described the cycle of ACEs (Dube 2020):
- Childhood adversity – abuse, neglect, and stressors in the home
- Adolescent outcomes – associated with substance use, suicidality, mental health, early pregnancy, substance misuse, and sexually harmful behaviour and exploitation
- Adult outcomes, associated with chronic diseases, substance use, obesity, STD/HIV risk, sexual risk behaviour, mental health, suicidality, emotional dysregulation
- Impact on Parenting – The cycle is completed through the association with harmful parenting which completes the cycle.
References
Dube S (2020). Twenty years and counting – the past, present and future of ACEs Research, in G. Asmundsen and T Afifie (eds). Adverse Childhood experiences. Academic Press.
Felitti V.J. Anda R.J et al (1998). Child Abuse and Household dysfunction and adverse health impact ACE. Am J Preventitive Med, 14: 245-258.
McLaughlin K et al (2016). Maltreatment Exposure, and the long shadow of adverse childhood experiences. Psychological Science Agenda.
Vizard, E., Gray, J., & Bentovim, A. (2021). The impact of child maltreatment on the mental and physical health of child victims: A review of the evidence. BJPsych Advances, 1-11. doi:10.1192/bja.2021.10.
Back to Contents
What we don’t know about ACEs
1. Measuring ACEs
As we have commented, the introduction of Adverse Childhood Experiences as a risk matrix has resulted in significant developments. The relationship has been demonstrated as robust, there are concerns that high levels of adversity associated with neurobiological traumatic responses may result in a harmful outcome. There is a growing awareness of the relationships, advocacy of regular screening in adult and young people, the introduction of Trauma-Informed approaches.
However there has been a growing awareness of limitations of the ACEs score, and the need to be aware of a wide range of adverse influences in the community, associated with health inequity, deprivation, racism, and disadvantage. There are concerns that the ACEs score has been ascertained retrospectively in many studies, and that the items of the ACEs score are not equal in relevance. A high ACEs score is associated with harmful outcomes on a population level, but is not associated with outcomes for the individual. The ‘Classical Ten’ ACEs has been extended to ‘Forty Aces’ when ACEs in children are studied directly.
Current evaluation of the uses of ACEs scores to measure adversity as an indicator has indicated that there is limited support for universal screening or routine enquiry utilising the ACEs score in childhood or adults. There is a need to define effective measures of adversity to predict future harm. There is growing research on the network of risk, resilience and vulnerability factors which need to be considered, when there are concerns about children and young people referred across services for children and young people.
We need to develop reliable ways of predicting health outcomes for the individual, a variety of approaches have been researched – using single forms of adversity, groupings by theoretical constructs, e.g. DMAP – threat or deprivation, or combinations of ACEs through Latent Class Analyses. Extending and operationalising the Assessment Framework developed for welfare contexts, across services may be a further approach to consider. We have described the potential value of a risk calculator approach as an alternative to the ACEs score.
2. The pathways to adult mental and physical ill-health
In the review of research on cases in the last 20 years we have noted that there has been a shift in emphasis from the original research of Felliti and colleagues (1998) which explored the association between childhood adversity and adult physical and mental health, Direct research on childhood and young people and the social context, together with longitudinal research has significantly enlarged our understanding of possible pathways from adversity to adult morbidity and mortality. Adversity and risk has to be balanced with resilience and vulnerability factors, from the individual, parenting, the family and community. This makes for a more nuanced understanding of potential pathways and associations with psychopathology and health. However, what remains unanswered is an understanding of the processes which drive the transformation.
A number of theories have been advanced including neurobiological responses to adversity. Traumatic responses have been researched including ‘Latent Vulnerabilities’, ‘Chronic Inflammatory Responses and ‘Allostatic ‘Wear and Tear’. Longitudinal Research shows promise in differentiating a variety of adversities, and outcomes – psychological, behavioural and neurobiologically. Further research is essential to find more effective ways of intervening to prevent ill health in identified vulnerable individuals.
3. The prevalence of ACEs
Another important area where we need to develop knowledge is to understand the prevalence of ACEs in the community. There is an extensive literature on the prevalence of the core forms of maltreatment, physical, sexual and emotional abuse and exposure to violence (Radford et al., 2011) and the overlap through the research on polyvictimisation (Finkelhor 2007). With the addition of a wide range of household dysfunctions such as parental mental health, substance abuse, separation, loss, divorces and community violence associated with different forms of adverse experiences, there is a a significant challenge to assess the prevalence of ACEs.
The work of the UC Health Equity Group has illustrated the relationship between deprivation and higher levels of ACEs providing a model for future research. The introduction of extensive screening tools based on epidemiological research by Turner and Finkelhor which includes a wide range of Adverse Experiences may assist researchers to determine the prevalence of Childhood Adverse Experiences in the community as part of a more extensive evaluation of children and young people’s development,
4. Intervention to modify and prevent the impact of ACEs
The challenge to effectively intervene to prevent the harmful impact of ACES when identified in childhood, and young people to prevent the associated morbidity, mortality and ill-health in adult life is considerable. The introduction of Trauma-informed approaches has the potential to transform the views and responses of the workforce in relation to the needs and responses of children and young people referred to mental health, safeguarding, offending and care services, and children and young people looked after or living in contexts of significant stress of adversity. It also has the potential to transform adult services to be aware of the adversities children and young people experience when parents have a variety of mental health difficulties, to be aware of the association between exposure to multiple adversity, and subsequent health.
However, the evidence for the effectiveness of these approaches, both short term and longer-term reduction of harmful psychological and physical health is limited, and at an early stage. Research on specific interventions for ACEs is limited to children under six years of age. Implementing the recommendation that there should be a focus on identifying and intervening with maltreatment in childhood is also challenging.
There is extensive research on intervening with single forms of maltreatment. However, there is limited research on overlapping multiple maltreatment. Trauma – Focused CBT being the one intervention which is associated with more favourable outcomes, and parenting interventions are effective.
Intervening with the many areas of potential adversity parental mental health, substance misuse violence in the home and the community is far more challenging and requires collaborative services. There is a need for further primary, as well as secondary and tertiary prevention activities, including strengthening communities and families, building resilience and support to provide trauma- informed services. (Gentry and Paterson, 2021)
A modular approach which provides a library of interventions derived from common treatment elements, can be integrated to meet complex needs children, parents, and families when significant adversities are identified. The approach works well in practice. Although it includes an effective model of intervention for mental health concerns of children and young people, further research is required to evaluate the effectiveness to reduce longer term morbidity and mortality.
Van IJzendoorn and colleagues (2020) conducted an umbrella synthesis of meta-analyses on child maltreatment antecedents and interventions. They concluded that there was now good evidence to identify parental risk factors for maltreatment. These risk factors include parents who have themselves been victims of child maltreatment, been subjected to interpersonal violence, had negative personality attributes associated with mental health disorders, and have limited social and material resources.
However, they noted there was a “‘power failure’ of interventions to prevent or decrease child abuse and neglect in the next generation, with the effect sizes for intervention being substantially smaller than the effect sizes for most of the antecedents of child maltreatment” (Van IJzendoorn et al., 2020, p. 283). They further commented,
“The scarcity of evidence-based means to break the circle of maltreatment is deplorable. Child maltreatment is a widespread global phenomenon affecting the lives of millions of children all over the world, which is a betrayal of the United Nations Convention on the Rights of the Child (United Nations, 1989)” (p. 284).
References
Finkelhor, D., Omrod, R. K., & Turner, H. A. (2007). Poly-victimisation: A neglected component in child victimization. Child Abuse and Neglect, 31, 7–26.
Radford, L., Corral, S., Bradley, C., et al. (2011). Child abuse and neglect in the UK Today. London: NSPCC. https://learning.nspcc.org.uk/media/1042/child-abuse-neglect-uk-today-research-report.pdf
Van IJzendoorn, M. H., Bakermans-Kranenburg, M. J., Coughlan, B., & Reijman, S. (2020). Differential susceptibility perspective on risk and resilience. Journal of Child Psychology and Psychiatry, 61(3), 272–290.
Adverse Childhood Experiences, Adverse Community Environments, climate change, the pandemic, the internet and refugee asylum seekers
1. A Pair of ACEs
One of the results of the introduction of ACEs was the observation that a common factor in the direct effects of adversity on children and young people was exposure to trauma and associated traumatic responses. ‘Toxic Stress’ was the term applied to exposure to prolonged stressful experiences. The neurobiological impact of traumatic and stressful events has been described as resulting in a “cascade of toxic stressful, inflammatory and hormonal responses with marked effects on brain morphology, function and network architecture” (Teicher, Samson, Anderson, & Ohashi, 2016, p. 254).
Complex adversity leads to clusters of symptoms and multiple different types of disorders rather than specific disorders – ‘trauma-related psychopathology’ (Lewis et al., 2019). A spectrum of overlapping internalizing and externalizing disorders results, as noted in the research of Meehan and colleagues. The specific response depends on their interaction with other risk and protective factors (McCrory, Gerin, & Viding, 2017), and the more extensive the adversity, the number of victimisations experiences the greater the severity of psychiatric symptoms (Cecil, Viding, Fearon, Glaser, & McCrory, 2017)
As a result many services have adopted a ‘Trauma Informed Focus.’ Pachter and colleagues (2017) described the development of a ‘Community-Wide Initiative to Address Childhood Adversity and Toxic Stress: A Case Study of The Philadelphia ACE Task Force”.
Gentry and Paterson (2021, p. 2) define Trauma Informed approaches:
Trauma informed: ‘A program, organization, or system that is trauma-informed realizes the widespread impact of trauma and understands potential paths for recovery; recognizes the signs and symptoms of trauma in clients, families, staff and others involved with the system; and responds by fully integrating knowledge about trauma into policies, procedures and practices, and seeks to actively resist re-traumatization’.
Rebeca Lacey and Helen Minnis in their 20 year review of ACEs noted,
Adverse Childhood Experience scores have been instrumental in stimulating innovations in practice. ACEs awareness promotion – data from population studies has increased public awareness, Trauma-Informed Training of front-line staff helps staff understand ’what has happened’ and consequences, with a resulting compassionate workforce, early intervention, integrated and collaborative services.
The illustration below gives an idea of the elements of an ACEs hub.
The structure and function of an ACEs hub

2. Relationship between ACEs and deprivation
Based on the evidence of potential harmful impact of ACEs, Hughes et al (2017) argue that ACE informed practice can (should) be developed across multiple settings:
- including schools,
- criminal justice agencies,
- social care assessments of children and their families
- when children are showing evidence of being subject to maltreatment, with associated parental mental health, substance abuse, or conflict.
Routine enquiry and service development
A programme of routine enquiry concerning the presence of ACEs has been advocated (REAch) and initiated to enable identification of need and early intervention or access to services. Routine enquiry of children and young people has been established in the State of California, and will provide important information about the approach and its value in reducing health concerns on a population level.
However, in a review of the value of routine enquiry from the Early Intervention Foundation, Asmussen and McBride (2021) conclude,
‘In our view all ACE universal screening activities should be stopped until robust testing and validation takes place. Additionally, practitioners should recognise that it is unlikely that ACE scores will ever represent an appropriate way of measuring individual risk or making treatment decisions. This means that ACE scores should never be used as a basis for treatment referral and, given the emerging evidence showing that many vulnerable individuals are less likely to answer ACE questionnaires truthfully, probably should not be used to initiate conversations with children and adults about difficult childhood histories’
Community Responses – Trauma-Informed Care
Services have come together to develop a community response. Integrated ACEs hubs have been developed in Scotland and Wales, and across a number of states in the US. Authorities across the UK are considering the need to develop a Trauma-informed Approach to planning and delivering services to children, young people and their families. These include children who are abused and neglected, sexually exploited, refugees, looked after, and those who have offended. In these contexts ACEs scores would need to be contextualised through information on a wide range of risk, resilience and vulnerability factors to make a holistic assessment.
Bendall and colleagues (2021) have conducted a systematic review and synthesis of trauma-informed care within outpatient and counselling health settings for young people. They found there was good evidence for the implementation of the approach, and improvement in trauma-informed knowledge, practice and collaboration but limited evidence of outcomes.
Research on the value of Trauma-informed Care
Asmussen and McBride (2021, p. 16) state that
‘While the principles underpinning trauma-informed care may be beneficial for improving practice, we are concerned that most trauma-informed activities have yet to be robustly evaluated’
‘Although Trauma focused practice is being widely adopted and advocated there is a need for further research to determine the effectiveness of the approach….and that government should fund a series of national evaluations aimed at investigating the benefits of trauma-informed care training for the frontline practitioners who are receiving it, including social workers, teachers, health visitors and the police’.
The evolution of trauma-informed care will require
- a clear consensus on the definition, principles, and components of trauma-informed care to create a uniform set of practice guidelines.
- instrumentation to measure its effectiveness and assess organizations to capture their degree of trauma-informed care and its link to client-level indices of well-being.
- methodologically rigorous studies to build the evidence base of trauma-informed care as a framework and complement to trauma-specific services; and,
- public and private support, at the federal, state and local levels, to fund research and implementation.
3. The Covid-19 pandemic as an Adverse Experience
The Health Inequity group based on the incidence studies of Bellis et al. (2014) have asserted that reducing ACEs would have a significant impact on harmful responses associated with ACEs – reducing early sex, unintended pregnancy, smoking, binge drinking, cannabis use, heroin crack use, violence victimisation, and perpetration, incarceration and poor diet. They advocate the importance of reducing the impact of social inequity as a pathway to improve the health of children young people and adults.

A public health approach to reducing ACEs is advocated as a key approach to reducing the impact of ACEs. Gentry and Paterson’s review (2021, p. 3) concluded that
Policy approaches to reducing child poverty/inequality have potential to reduce ACEs. Prospective cohort and cross-sectional studies suggested family, institutional and community support were associated with fewer adverse outcomes. Peer-led home visiting programmes using volunteer or paraprofessional home visitors from the local community could support parenting and attendance at healthcare appointments compared with standard community maternal-child care (Walsh et al., 2020).
Asmussen and McBride (2021, p. 19) in their Delphic survey of professionals reported a consensus that
- The UK government should adopt a public health approach which explicitly aims to prevent child maltreatment from conception to age 18.
- ‘Specifically targeting child maltreatment may be a particularly effective way of improving the lives of vulnerable children, including those who have experienced multiple ACEs .
- Evidence-based parenting support should be made available at the universal, targeted and individual level as a first step in a population-wide strategy for preventing and reducing ACEs. a sustainable whole- system strategy needs to be developed in every community to prevent and reduce ACEs at the population level.
- We have noted the alliance to stop the corporal punishment of children and young people. There is an extensive literature on prevention of sexual abuse and violence through school’s programmes, and there is evidence that a ‘blended’ prevention approach through introducing Triple P Parenting at a primary level through public education – video – and secondary and tertiary levels through more direct work, reducing the incidence of abuse and neglect (Prinz 2009).
4.The impact of climate change on mental health and emotional well-being
Whilst there is an extensive literature associated with modifying the impact of abuse and neglect e.g. Macdonald et al. (2016) described 162 studies and 66 controlled trials.
Marie-Mitchell and Kostolansky (2019) were able to identify 20 Randomised Control Trials which focused on ACEs. The studies all focused on children under five years of age.
- The commonest ACE was parental mental health; there were fewer parent alcohol, substance abuse or domestic violence associated ACEs studied
- Multicomponent medium- to high-intensity interventions that utilized professional home visitors to provide parenting education or mental health counselling demonstrated the largest effects. There was evidence of reduction of the impact of ACEs and improved parent-child relationships.
- However, there was no research which included children older than 6 years of age, or on improving child outcomes for other ACEs
- We have emphasised the importance of researching the effectiveness of the Trauma -Informed model of Intervention.
5. Exposure to harmful influences online
The Framework for the Assessment of Children in Need and their Families (the ‘Assessment Framework’) (Department of Health et al., 2000) was introduced as part of the process of enlarging the field of vision of professionals concerned with children in need of services, as well as in need of protection. This eco-systemic framework provides a conceptual map to help professionals consider the child’s functioning and needs, the capacity of parents to provide for those needs, the way their needs were being met (or not) and the role of family and environmental factors on the child or the parenting capacity of their caregivers. The approach was intended to extend professional practice from a narrow focus on ‘risk assessment’ and protection to a broader holistic consideration of the child and their family and the context in which they lived, to raise the standard of professional understanding of needs and to focus interventions more effectively. The approach is a parallel to the development of the concept of Adverse Childhood experiences which includes forms of maltreatment and the family context.
The Assessment Framework is underpinned by a series of principles that emphasise the centrality of the child, that an understanding of child development is critical to working with children and their families, the importance collaboration with children and their families, placing an emphasis on identifying strengths as well as difficulties and the influence of environmental factors on parent’s capacities to respond to their child’s needs.
A series of tools and approaches were identified and developed to support the implementation of the Assessment Framework for use by a range of practitioners from different professional and voluntary backgrounds and with differing levels of experience and expertise.
Identification of abuse and neglect, assessment, and analysis
The assessment tools included the Family Pack of Questionnaires and Scales (Cox and Bentovim, 2001) which included tools to gather information about emotional and behavioural difficulties in both children and adults, parenting problems, recent life events, mental health difficulties, alcohol problems, and the quality of family life; the HOME Inventory UK Approach (Cox et al., 2008; Cox and Walker, 2002) which was originally developed as a research tool in the USA (Caldwell and Bradley, 2001) and assesses the quality of parenting and the home environment provided for a child using a semi-structured interview schedule; and the Family Assessment (Bentovim and Bingley Miller, 2002; 2012) which enables practitioners to assess family functioning and family relationships, including parenting, and the impact of family history.
The Safeguarding Children Assessment and Analysis Framework (SAAF) (Bentovim et al., 2009; Pizzey et al., 2016) was developed to assist practitioners make an analysis of the information gathered using the assessment tools. The SAAF makes a systemic analysis of the strengths (protective and resilience factors) and difficulties (risk and harm factors) identified from the assessment, provides a prediction of the likely outlook for the child if nothing changes, assesses the prospects for successful intervention and provides the evidence for the plan of intervention. The Safeguarding Children Assessment and Analysis Framework assessed in a RCT by Macdonald et al. (2017).
An intervention approach, the Hope for Children and Families Modular Approach (Bentovim et al., 2021; Bentovim and Gray (eds)., 2016; 2017; 2018) was designed to meet complex needs associated with child abuse and neglect, and is relevant to intervention to prevent the associated harm of ACEs.
The assessment framework domains and dimensions

The definition of Child in Need is set out in Section 17 of the Children Act 1989 and was operationalised in the Assessment Framework. The elements Felliti et al. (1998) introduced can be mapped on to the dimensions of the Assessment Framework, including parental mental health, parenting capacities, and an extensive description of strengths and difficulties across the framework – a potential approach to make a holistic assessment when there are concerns about children and young people presenting across services.
6. The Hope for Children and Families Modular Programme
The limitations of current intervention approaches to modify the harmful impact of ACE (Bentovim et al., 2021)
Despite the availability of a wide range of effective evidence-based interventions to prevent the harmful effects of adversity, there is limited and patchy use of these interventions to address the needs of individuals who have experienced extensive exposure to ACEs with the complex mental health impacts, and the cumulative harmful impact on the developing child’s mental health and wellbeing.
The NICE guidance (2017) on intervention invites practitioners and commissioners to consider utilising about 15 evidence-based manualised approaches for specific forms of child maltreatment from different theoretical approaches (psycho-dynamic, systemic, and cognitive-behavioural). These are to be delivered in the home or office, for a range of parenting relationships (birth, foster or adoption) and developmental stages of children. The importance of being trained in the relevant approaches is stressed.
These approaches include:
- Enhanced Triple P programme, UK Department of Health’s Healthy child programme and Parents under Pressure for early help contexts
- Attachment-based interventions, e.g. Attachment and Biobehavioural Catch-Up, and child-parent psychotherapy for physical or emotional abuse or neglect of children under 5
- SafeCare and parent-child interaction therapy for physical or emotional abuse or neglect for children up to the age of 12
- Multi-systemic therapy for child and abuse (MST-CAN) for adolescents aged 10 to 17
- Trauma-focused cognitive behavioural therapy, individual psychoanalytic therapy, group psychotherapeutic and psychoeducational sessions for sexual abuse where there is evidence of anxiety, sexualised behaviour or PTSD symptoms.
In general, these are well evidenced approaches, which will be helpful to services for children aged 0-5 years, looked after children and sexually abused children and adolescents, and specialist services. It is recognised that the most effective interventions working with maltreated children draw on differing theoretical models and concepts. However, in practice, implementation of such a complex set of evidence-based approaches presents a considerable challenge to planners and commissioners of services because both practitioners and their managers need training and supervision in the different approaches mentioned above and elsewhere.
Macdonald et al. (2016) comment that Trauma-Focused Cognitive Behavior Therapy is the most effective for post-traumatic stress disorder, complex trauma, and associated emotional problems. However, “most children experience more than one form of maltreatment, and there is growing recognition of the need to better take into account children’s profiles of maltreatment in order to improve policy and practice” (p. 38). The complexity of an individual’s responses to multiple ACEs, therefore, demands a therapeutic approach that can encompass an infinite range of responses.
How a modular intervention approach may help
Modular approaches were developed to meet the treatment needs of children and young people with a range of overlapping mental health problems (e.g., Chorpita, Daleiden, & Weisz, 2005). The approach capitalized on the knowledge embedded in evidence-based treatments for mental health (e.g., Chorpita & Daleiden, 2009). A structured methodology was developed to map, identify and categorise the common treatment features from 615 treatments in 322 randomized trials. It was possible to distill out the specific practice components of each type of treatment i.e. practice elements from different manuals.
The Modular Approach for Children with Anxiety, Depression, Trauma and Conduct problems (MATCH-ADTC: Chorpita & Weisz, 2009) is a multi-disorder intervention system that incorporates treatment procedures (elements) and treatment logic (coordination) based on four successful evidence-based CBT interventions for childhood anxiety, depression, trauma (TF-CBT), and conduct problems, with modifications allowing the system to operate as a single protocol. The approach was more effective in improvements in a wide range of mental health problems, than using the component manuals.
The Hope for Children and Families Intervention Resources
Building on the MATCH-ADTC in collaboration with Chorpita and colleagues, common treatment elements were distilled from across the field of interventions for individual forms of child maltreatment, Twenty-two RCTs were identified for the treatment of different forms of maltreatment (Bentovim & Elliott, 2014). The forty-seven common practice elements that emerged were categorized as focusing on work with children, young people, parents/caregivers and the family as a whole, and were added to the MATCH-ADTC to create a library of modules which can be integrated into a management plan, establishing collaborative goals, with children and families, and can be adapted for use across services.
Elements targeting the antecedents of adverse childhood experience include psychoeducation for parents; exploration of the impact and origins of abuse and exposure to violence; addressing parental mental health difficulties; and learning positive parenting skills.
The elements targeting work with children and young people include psychoeducation on the impact of their maltreatment; managing and exposing traumatic thoughts and feelings; relaxation; problem-solving; relationship building; and, social skills talent/skill building. Modules are gathered into a set of guides organised around the Assessment Framework Triangle.

Guides
Each of the guides is described below.
Engagement and Goal Setting
The ‘Engagement and goal setting guide’ (Bentovim et al., 2017) helps practitioners promote a sense of hopefulness, orientates the practitioner and family to the profile of Adverse Childhood Experiences, family strengths and difficulties, and establishes shared goals, and the measures by which outcomes will be monitored.
Targeting the parental antecedents of maltreatment and ACEs
Four intervention guides cover different areas of parenting: ‘Promoting positive parenting’ (Roberts, 2016), ‘Promoting children and young people’s health, development and wellbeing’ (Bentovim, 2017a); ‘Promoting attachment, attuned responsiveness and positive emotional relationships’ (Gates & Peters, 2017); and, ‘Modifying abusive and neglectful parenting’ (Bentovim, 2017b). The guides’ modules provide an understanding of the historical and familial stresses associated with ACEs -abusive and neglectful parenting; the impact of abuse and neglect on children’s health and development; interrupting and modifying abusive and neglectful processes, modifying negative perceptions of children, and improving the standard of care. They can be adapted for use with foster, adoptive, and residential caregivers.
Working with families
The ‘Working with Families’ intervention guide (Jolliffe, 2016) supports practitioners in their work with families as a group, and in various combinations. This skill helps them to facilitate parent-child communication, and interrupt and find alternatives to conflict within the family, and between the parents and community.
Direct work with children and young people
Two intervention guides consider working with children and young people: ‘Addressing emotional and traumatic responses’ (Weeramanthri, 2016); and, ‘Addressing disruptive behaviour’ (Eldridge, 2017). These are core guides for working with children and young people who have been subject to ACEs. These modules help practitioners work with parents and caregivers to develop children and young people’s generic skills to manage their emotions, be safe and develop problem solving abilities. Once basic coping skills have been mastered there are modules for addressing specific anxiety, mood, traumatic responses and disruptive behaviour.
Working with child sexual abuse
The ‘Working with child sexual abuse’ guide (Eldridge, 2016) considers working with children and young people who have been abused sexually, their parents/caregivers, and with those who are responsible for or who display harmful sexual behaviour. It is essential that practitioners develop skills to support children and young people who have been exposed to sexual abuse and demonstrate sexually harmful behaviour, often in association with other forms of maltreatment and adversity, and to support their parents.
Effectiveness of the HfCF
The piloting and subsequent implementation of the program have demonstrated that the HfCF Intervention guides for practitioners could provide effective resources for use within different types of children’s services provision (e.g., social care/child protection, health, education, and youth justice services), and at all stages of the therapeutic process. They proved helpful for a range of services – intervening early and targeting vulnerable families, to responding to identified maltreatment, and working with children placed in foster care, residential or adoptive placements.
The HfCF resources could provide the tools to deliver effective Trauma-Informed Practice, to address the impact on children’s health and behavior of multiple ACEs across different agencies in the community. Modular approaches have proven effective in RCTs for children and young people with overlapping mental health disorders and have proven valuable to practitioners. However, the effectiveness of the HfCF has not yet been tested for polyvictimization and multiple ACEs through a RCT.
Relevance to Child and Adolescent Mental Health
It is estimated that over 40% of Children’s and Adolescents’ mental health problems are associated with adversity, demonstrated strikingly during the pandemic as a source of significant adversity. Research to prevent harmful impacts is a key challenge for our field.
References
Allen M & Donkin A (2015) The impact of adverse experiencesin the home on the health of children and young people, and inequalities in prevalence and effects. Institute of health equity: London, UCL.
Asmussen K., Fischer F., Drayton E. et al. (2020). Adverse childhood experiences. What we know, what we don’t know, and what should happen next. London: Early Intervention Foundation.
Asmussen K and McBride T (20210 Adverse Childhood Experiences – Building Consensus – What Happens Next. London; Early Intervention Foundation.
Bendall S, Eastwood O, Cox G et al. (2021) A systematic review and synthesis of trauma-informed care within outpatient and counseling health settings for young people. Child Maltreat 2020;1077559520927468. (2nd July 2021, date last accessed).
Bentovim, A., Cox, A., Bingley Miller, L. and Pizzey, S. 2009. Safeguarding Children Living with Trauma and Family Violence: A Guide to Evidence-Based Assessment, Analysis and Planning Interventions. London: Jessica Kingsley.
Bentovim A (2017a). Promoting children and young people’s health, development and wellbeing. In A Bentovim & J Gray (eds.). Hope for Children and Families: Building on strengths, overcoming difficulties. York, UK: Child and Family Training.
Bentovim A (2017b). Modifying abusive and neglectful parenting. In A Bentovim & J Gray (eds.). Hope for Children and Families: Building on strengths, overcoming difficulties. York, UK: Child and Family Training.
Cox, A. & Bentovim, A. (2000). The Family Pack of Questionnaires and Scales. London:The Stationery Office.
Cox, A., Pizzey, S. & Walker, S. (2009). The HOME Inventory: A Guide for Practitioners – The UK Approach. York, UK: Child and Family Training.
Cox, A. & Walker, S. (2002). The HOME Inventory: A Training Approach for the UK. Brighton: Pavillion.
Bentovim A, Chorpita BF et al (2020). The value of a modular, multi-focal, trauma-informed therapeutic approach to preventing child maltreatment: hope for children and families intervention resources. A disruptive innovation. Child Abuse & Neglect 119:104703.
Bentovim A & Gray J (eds.) (2016; 2017; 2018). Hope for children and families: Building on strengths, overcoming difficulties. York, UK: Child and Family Training.
Bentovim A, Gray J, Heasman P & Pizzey S (2017). Engagement and goal setting. In A Bentovim & J Gray (eds.). Hope for Children and Families: Building on strengths, overcoming difficulties. York, UK: Child and Family Training.
Caldwell, B. M. and Bradley, R. H. (2001) Home Observation for Measurement of the Environment: Administration Manual (3rd edition). Arkansas: University of Arkansas.
Cecil, C.A.M., Viding, E., Fearon, P., Glaser, D., & McCrory, E.J. (2017). Disentangling the mental health of childhood abuse and neglect. Child Abuse and Neglect, 63, 106-119.
Chorpita BF & Daleiden EL (2009). Mapping evidence-based treatments for children and adolescents: Application of the distillation and matching model to 615 treatments from 322 randomized trials. Journal of Consulting and Clinical Psychology, 77(3): 566–579.
Chorpita BF & Weisz JR (2009). Modular approach to children with anxiety, depression, trauma and conduct Match-ADTC. Satellite Beach FL: PracticeWise LCC.
Chorpita BF, Daleiden EL & Weisz JR (2005). Identifying and selecting the common elements of evidence based interventions: A distillation and matching model. Mental Health Services Research, 7: 5–20.
Chorpita, B. F., Daleiden, E. L., Park, A. L., Ward, A. M., Levy, M. C., Cromley, T., … Krull, J. L. (2017). Child STEPs in California: A cluster randomized effectiveness trial comparing modular treatment with community implemented treatment for youth with anxiety, depression, conduct problems, or traumatic stress. Journal of Consulting and Clinical Psychology, 85(1), 13–25.
Cox, A. & Bentovim, A. (2000). The Family Pack of Questionnaires and Scales. London:The Stationery Office.
Cox, A., Pizzey, S. & Walker, S. (2009). The HOME Inventory: A Guide for Practitioners – The UK Approach. York, UK: Child and Family Training.
Cox, A. & Walker, S. (2002). The HOME Inventory: A Training Approach for the UK. Brighton: Pavillion.
Department of Health, Department for Education and Employment, & Home Office (2000). The framework for the assessment of children in need and their families. London, UK: The Stationery Office.
Eldridge H (2017). Working with children and young people: Addressing disruptive behaviour. In A Bentovim & J Gray (eds.). Hope for Children and Families: Building on strengths, overcoming difficulties. York, UK: Child and Family Training.
Gates C & Peters J (2017). Promoting attachment, attuned responsiveness and positive emotional relationships. In A Bentovim & J Gray (eds.). Hope for Children and Families: Building on strengths, overcoming difficulties. York, UK: Child and Family Training.
Marie-Mitchell A & Kostolansky R. (2019). A systematic review of trials to improve child outcomes associated with adverse childhood experiences. American Journal of Preventive Medicine 56(5): 756–764.
Macdonald, G., Lewis, J., Ghate, D., Gardner, E., Adams, C. & Kelly, K. (2017). Evaluation of the Safeguarding Children Assessment and Analysis Framework (SAAF). London: Department for Education.
Macdonald G, Livingstone N et al (2016). The effectiveness, acceptability and cost-effectiveness of psychosocial interventions for maltreated children and adolescents: An evidence synthesis. Health Technology Assessment, 20(69), 1–508.
McCrory, E., Gerin, M. I., & Viding, E. (2017). Child maltreatment. Latent vulnerability, and the shift to preventative psychiatry – The contribution of functional brain imaging. Journal of Child Psychology and Psychiatry, 58, 338–357.
National Institute for Health and Care Excellence. (2017). NICE guideline. Child abuse and neglect.
NHS Highlands (2018). Adverse childhood experiences, resilience and trauma informed care: A public health approach to understanding and responding to adversity. Annual Report of the Director of Public Health 2018, NHS Highland.
Pachter, L., Lieberman, L., Bloom, S., & Fein, J.A. (2017). Developing a Community-Wide Initiative to Address Childhood Adversity and Toxic Stress: A Case Study of The Philadelphia ACE Task Force. Academic Pediatrics, 17(7), S130–S135.
Pizzey, S., Bentovim, A., Cox, A., Bingley Miller, L. and Tapp, S. (2016). The Safeguarding Children Assessment and Analysis Framework. York: Child and Family Training.
Prinz, R. J., Sanders, M. R., Shapiro, C. J., Whitaker, D. J., & Lutzker, J. R. (2009). Population-based prevention of maltreatment. Prevention Science, 10, 1–12.
Radford, L., Corral, S., Bradley, C., et al. (2011). Child abuse and neglect in the UK Today. London: NSPCC.
Roberts R (2016). Promoting positive parenting. In A Bentovim & J Gray (eds.). Hope for Children and Families: Building on strengths, overcoming difficulties. York, UK: Child and Family Training.
Walsh MC, Joyce S, Maloney T, Vaithianathan R. (2020) Exploring the protective factors of children and families identified at highest risk of adverse childhood experiences by a predictive risk model: an analysis of the growing up in New Zealand cohort. Child Youth Serv Rev 1;108:104556.
Weeramanthri T (2016). Working with children and young people: Addressing emotional and traumatic responses. In A Bentovim & J Gray (eds.). Hope for Children and Families: Building on strengths, overcoming difficulties. York, UK: Child and Family Training.
Back to Contents
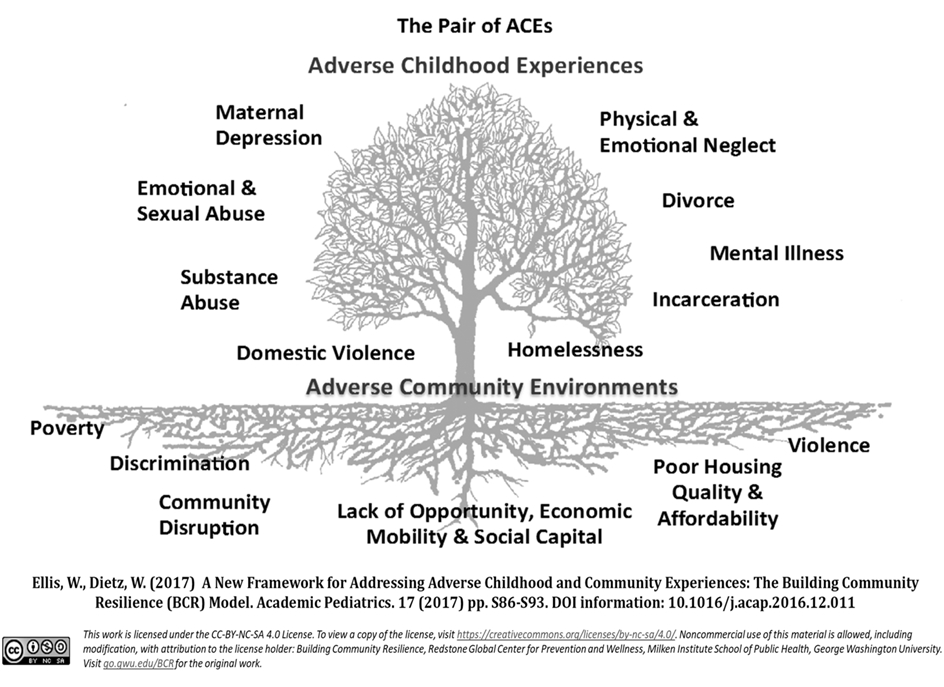
1. A Pair of ACEs
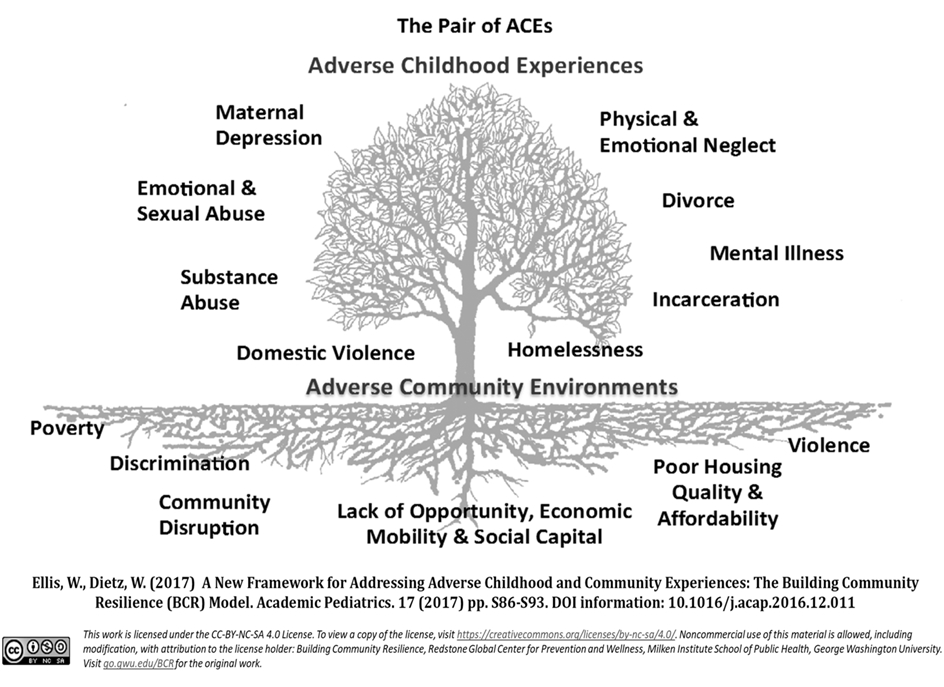
Ellis and Dietz in 2017 introduced a framework to address ACEs by describing ACEs in the context of Adverse Community Environments, a model which can be extended to include the impact of climate change and the Pandemic as potentially adverse experiences.
The tree describes the 10 Classic ACEs described by Fellitti et al., and the soil which ‘nurtures’ adversity includes Poverty, Discrimination, Community Disruption, Lack of opportunity, mobility and Social Capital, Poor Housing Quality, and Affordability, and Violence in the community.
This approach to putting in context represents more recent research on ACEs – direct research on children and young people, and research on the social context.
2. Relationship between ACEs and deprivation
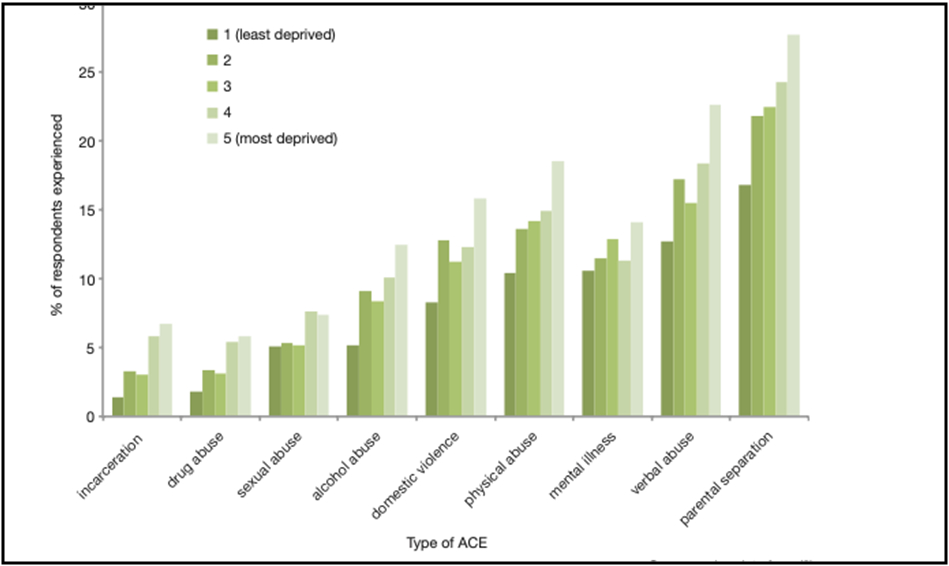
Michael Marmot’s UC Health Team (Allen and Donkin, 2015) noted in an extensive review of the prevalence of ACEs across communities, that those communities with the highest index of deprivation also had the highest incidence of individual ACEs. Parental separation was experienced by the highest number of respondents, followed by verbal abuse, mental illness, physical abuse and domestic violence.
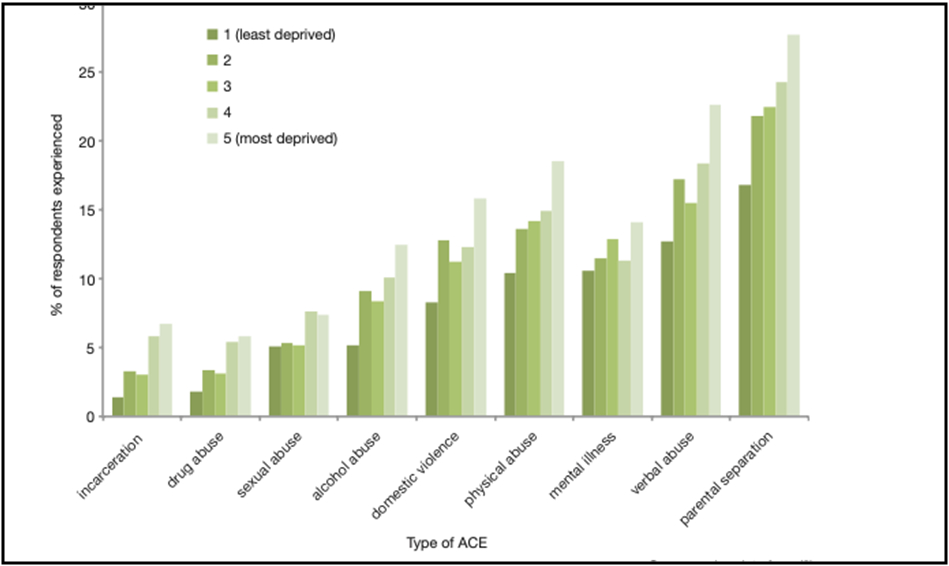
It is striking to note the role of environment stress reinforcing parenting and family stress. The Health Equity group advocates a model to understand the responses associated with high levels of adversity in childhood which includes the social context as stressors – poverty, social isolation, and protection policies, parenting and family factors, and social determinants – education and income.
The Health Equity Group has advocated the need for community intervention to ‘Build back Better’ in the face of the impact of deprivation in communities, a recommendation reinforced with the evidence of higher rates of Covid infections in deprived communities, associated with higher levels of adversity.
3. The Covid-19 pandemic as an Adverse Experience
There has been universal concern about the pandemic as an Adverse Experience which has affected whole populations. Adverse factors associated with harmful health outcomes, have also been noted by the Health Equity Group to be associated with worse outcomes of Covid infections.
There have been enormous economic and social shifts. Families have been living in virtual confinement coupled with massive economic disarray. There has been an increase in Domestic Violence and Substance Misuse. These are ideal conditions for a rise in children’s experience of abuse and neglect, with the reduction of contacts with those in the outside world who would see and identify harmful incidents.
A recent study (NHS Digital, 2020) of the mental health of children and young people In July 2020 during the COVID-19 pandemic concluded:
- One in six (16.0%) children aged 5 to 16 years were identified as having a probable mental disorder, increasing from one in nine (10.8%) in 2017. The increase was evident in both boys and girls.
Ford and colleagues (2021) noted there was a higher rate of admissions of younger children to hospital with self-harming behaviour
- There was a striking increase in eating disorders
- There was an increased rate of such responses when parents have mental health problems, family functioning difficulties and financial hardships
There was also an increase when children have ASD or ADHD which acted as a vulnerability factor.
The impact of the Pandemic as a universal Significant Adverse Experience depends on a number of associated factors -for example when there are other risk factors – e.g. associated with deprivation, and limited resoience factors.
4. The impact of climate change on mental health and emotional well-being
With increasing concern about Climate Changes as a significant Environmental Adversity Lawrence et al. (2021) from the Institute of global health innovation – Grantham Institute have described the environmental adversity as climate changes manifested as – Heat and droughts, wildfires, smoke, storms and flooding, rising sea levels, associated with negative mental health and emotional wellbeing of people around the world. This is manifested as:
- Increased suicides; severe distress following extreme weather events; provision of care disrupted
- Distress among young people and ‘eco-anxiety’
- The exacerbation of social inequalities, associated costs are often unaccounted for, underestimated, and hidden!!
5. Exposure to harmful influences online
Vizard et al. (2021) noted learning online and developing a wide range of IT skills is now the norm for many children in Western society. There are potential substantial benefits for all children and particularly those with special needs. Acquiring online skills, including competence at certain video games, may have offline social and educational benefits. These new skills could directly enhance the physical, emotional and social development of children with special needs in particular. Young people have embraced the internet and social media which has a powerful impact sometimes organising on their lives, self-images, entertaining, gaming, connecting and learning. Important issues such as the identification of young people’s gender as male or female can be debated.
However, the online world is not always a positive and safe environment for children, since potential predators are also online, seeking access to victims of all ages, there are risks of children being groomed for abuse, e.g. images of the sexual abuse of children, the entrapment of children to circulate images, falsification of identities as a way of meeting and exploiting children sexually. There is potential for children and young people to abuse other children and young people, cyber-bullying, attacking, and excluding which can trigger and maintain traumatic responses, associated with self-harm and suicidal responses (Vizard et al. 2021).
Children from all backgrounds can view harmful or outright abusive material online via live streaming sites. Parents in ‘safe’ families may be unaware of the nature of the material being viewed by their children. Exposing children and young people to sexually explicit material may be part of a ‘grooming’ process of the victim leading to direct sexual abuse (NSPCC, 2020).
Unsupervised access to violent and sexualised video games online may ‘desensitise’ a child or young person to the images and behaviour within the game. They may become increasingly determined to play the game up to certain ‘levels’, the repetition of which can lead to a form of addiction.
There is also a potential for the internet to act as force to promote health and wellbeing. Sites which focus on anorexic and self-harm can give adolescents and young people information which reinforces harmful behaviour, self-harming tendencies, such sites can also be helpful, provide informal support, and deliver on -line therapeutic interventions. The issue of safety of the internet, helping children, young people and parents understand the harmful and risks associated, and manage their children and young people’s internet use are constant themes.
6. ACEs in child refugee and asylum-seeking populations
(Ward et al., Public Health Wales, 2020)
The University team in Bangor have gathered the evidence together to demonstrate the significant level of ACEs in child refugees and asylum-seeking populations. In addition to ACEs within the home or family, are added the set of ACEs pre-migration – destruction, deprivation, witnessing and experiencing violence, during the migration journey, and post-migration. This is an example of taking a highly stressful context for children and young people, understanding the adversities children and young people might experience, to assist practitioners helping children and young people process those experiences and develop resilience and coping.

Von Werthern and colleagues (2019) have noted in the case of unaccompanied refugee minors, it is clear that a young person on the move from one hostile country to another over months or years cannot develop a secure sense of self-identity without a stable home background, a peer group to relate to and a sense of roots and belonging. At the very least this is a serious neglect of the young person’s emotional and social development.
Conclusion
This brief review of the contextual factors which are associated with significant adversity in children and young people’s lives associated with harmful health and development has significantly enlarged our understanding of ACEs as a concept. There are significant challenges to mitigate harmful effects on children and young people’s associated with deprivation, community violence, climate change, ,the refugee and asylum seeking, and the internet!!
References
Afifi T et al (2017). Spanking and adult mental health impairment: The case for the designation of spanking as an adverse childhood experience. Child Abuse & Neglect, 71: 24–31.
Allen M and Donkin A (2015). The impact of adverse experiences in the home on the health of children and young people, and inequalities in prevalence and effects. Institute of health Equity, UCL.
Ellis, W.R., & Deitz, W.H. (2017). A new framework for Addressing Adverse Childhood and Community Experience: The building Community Resilience Model. Academic Pediatrics, 17(7S), S86-S93.
Ford T et al (2021). Recent studies of health disorders in children and young people during the pandemic. BMJ 372: n614.
Lawrence E et al (2021). The impact of climate change on mental health and emotional well-being, implications for policy and practice. Institute of global health innovation – Grantham Institute.
NHS Digital (2021). Mental health of Children and Young People in England
NSPCC (2020). Protecting children from online abuse (last updated 23 Dec 2020). NSPCC Learning.
Wood S, Ford K, Hardcastle K, Hopkins J, Hughes K and Bellis M (2020) ACEs in child refugee and asylum-seeking populations. Public Health Wales.
Vizard, E., Gray, J., & Bentovim, A. (2021). The impact of child maltreatment on the mental and physical health of child victims: A review of the evidence. BJPsych Advances, 1-11. doi:10.1192/bja.2021.10
von Werthern M, Grigorakis G, Vizard E (2019) The mental health and wellbeing of unaccompanied refugee minors (URMs). Child Abuse and Neglect, 98: 104–46.
Back to Contents
Studying ACEs in Childhood Directly; Increased numbers of Adverse Childhood Experiences, offending behaviour, suicidal ideation and children in foster care
1. Direct research with children and young people
Finkelhor et al. (2012) pointed out that much of the original research focused on retrospective information and was limited to the Classic Ten Adverse Experiences. Predictors missing from the ACE study model were peer rejection, exposure to violence outside the family, low socio- economic status, and poor academic performance. Using an adapted form of their Juvenile Victimisation Questionnaire, Finkelhor et al. added to the original ACEs form.
2. Forty forms of Adverse Experiences
Subsequently Heather Turner working with David Finkelhor (International Journal of Child Abuse and Neglect, 2020), described 40 forms of Adverse Experiences which better predicted traumatic responses in childhood. These ACEs were derived from their epidemiological research on adversities experienced during childhood. They also developed screening questionnaires for use with parents for younger children, and questionnaires for use directly with young people.
The forty Adverse Childhood Experiences (ACEs), were assessed under 11 different conceptual domains, to predict trauma in childhood:
- Family instability – e.g., divorce homelessness
- Family disorder – e.g., mental health, drug, alcohol
- Interpersonal loss – e.g., death, illness, suicide
- Natural disaster – e.g., fire, flood, pandemics
- Economic stress – e.g., job loss, welfare
- Child-maltreatment – e.g., physical, sexual abuse
- Exposure to community violence
- Threatened serious assault, racial, homophobia,
- Physical assault
- Sexual victimisation – e.g., direct or on-line
- Peer bullying – e.g., cyber-bullying.
A different set of 15 items was associated with trauma symptoms for younger (2−9 year-old) compared to older (10−17 year-old) youth.
Physical and emotional abuse proved important for both age groups.
However, family-related factors were associated with trauma symptoms in younger children, while community and peer violence exposures were more relevant for older children.
3. A National Traumatic Stress Survey
Dierkhising et al. (2019) carried out an analysis of a longitudinal study of health outcomes associated with multiple adversity. They concluded:
- Exposure to multiple adversity from early childhood to middle childhood, and adolescence represents cumulative trauma exposure which is associated with higher scores – Internalizing, Externalizing, and PTSD symptoms
- Early childhood adversity is associated with both internalizing and externalizing problems
- Recent adversity in adolescence, is associated with internalizing problems –anxiety and depression in adolescence, and is also associated with self- harming behaviour.
This research has added to the findings of the association between adversity and mental health responses, noting the differential associations between early and later adversities.
4. The harmful effects of ACEs associated with children and young people in conflict with the law
The studies reviewed above have indicated that Externalising Disruptive behaviours are a characteristic response associated with cumulative adversities, and large-scale studies of young people who have been referred for offending behaviour has confirmed the association with ACEs.

There is a higher prevalence rate of adversity and trauma compared to population studies (Baglivio and Epps et al., 2014; Dierkhising et al., 2013). The figure shows that juvenile offenders are more likely to have associations with four or more ACEs than the study population. These responses may be associated with intellectual disabilities, emotion dysregulation and out-of- control behaviours, antisocial behaviour which is associated with involvement in the criminal justice system (Vizard, 2013; Walsh 2018, p. 18). Vizard also draws attention to the cycle of traumatic effects of a young person’s own sexual or violent behaviour on themselves, on their child victims and on assessing and treating professionals.
Other findings include.
- Multiple forms of trauma are more likely
- Higher ACEs also associated with higher likely of re-offending.
- There are also protective factors operating which mitigate against the association.
- The Cambridge longitudinal study (Craiga et al., 2017) noted young people who had been subject to multiple ACEs were less likely to offend if they also had high school attainment, low daring, low hyperactivity, low impulsivity low neuroticism, low dishonesty, and low troublesomeness
- Those individuals who have a Life-course-persistent antisocial trajectory experienced extensive adversity associated with brain cortex differences.
5. Suicidal ideation and adversity
Some of the most concerning situations are young people who self- harm, or display suicidal preoccupations, and suicide attempts. Longitudinal research with young people has explored the association between adversities and subsequent self-harming behaviour.
The Longscan study (Thompson et al., 2012) notes that cumulative lifetime adversities are associated with teen suicidal ideation. Life-time adversities include maltreatment, emotional and sexual abuse, witnessing violence, parental mental health, and residential instability, separations.
- Aged 16 each additional ACE led to 11% was associated with likelihood to report self-harm.
- Recent high adolescent adversity –maltreatment and high peer stress, face to face and cyber-bullying, was also associated with suicidal ideation, poor health, somatic complaints, and any health problem (Carbone et al., 2021).
- High ACEs – generally were associated with lower educational attainments, depression, smoking drug use and obesity.
- Girls were significantly more likely to report suicidal ideation than were
The Avon Longitudinal Study of Parents and Children has been studied to establish predictors of future suicidal and self-harm (Mars et al., 2019) Among participants with suicidal thoughts, they found that the
‘ strongest predictors of transition to attempts, – non-suicidal self-harm, cannabis use, other illicit drug use, exposure to self-harm, and higher levels of the personality type intellect/openness. Among participants with non-suicidal self-harm at baseline, the strongest predictors were cannabis use, other illicit drug use, sleep problems, and lower levels of the personality type extraversion’.
These findings indicate the importance of using longitudinal, prospective studies to establish further understanding between adversity and specific outcomes.
6. Traumatic experiences of foster care and children and young people
Research by Lehman et al., (2020) focused on significant adversities reported by children and young people in foster care in Norway. This is an example of research on a specific population of children and young people in alternative care and examines the association between the complex trauma. Many of these young people were exposed to Post- Traumatic Stress Disorders and Attachment Disorders.
Traumatic experiences
Traumatic events
- Involved in a serious accident – 13%
- Experienced terror or war 1%
- Injury, sickness, sudden death of loved ones 54%
- Experienced bullying or threats 24%
- Abduction, kidnapping 6%
- Hit, kicked, pulled, injured, threatened outside family 25%
- Witnessed others outside family being kicked, pulled, injured, ridiculing, attacking each other 36%
- Confusion or helplessness 27%
|
Any Abuse 36%
- Witnessing parents or other grown-ups being injured or threatened 16%
- Kicked, injured, threatened by a parent 18%
- Being sworn at, offended, and ridiculed 24%
Any Neglect 36%
- Cared for a parent 15%
- Felt unloved, not taken care of, not enough to eat, wearing dirty clothes, caring for siblings 23%
Any Sexual Abuse 24%
- Sexual abuse pictures taken 6%
- Touching, force to touch 13%
- Attempted intercourse 6%
|
Half of the 302 Norwegian children and young people showed symptoms of PTSD, and a significant proportion demonstrated
- reactive attachment disorders B Type – Low social responsiveness/ emotional dysregulation – significant association
- DSED – Disinhibited social engagement disorder – significant association
It was noted there was a similarity in these response to Complex PTSD which is characterised by ‘Disturbances in Self-Organization’ (DSO), dysregulated affects, a negative self-concept, and disturbed relationships. This research extends the growing number of direct research studies exploring potential pathways from adversity to significant psychopathology.
7. The impact of neglect
A core dimension of ACEs is neglectful care associated with many forms of adversity. When combined with threat there is a significant cumulative impact. The impact of neglect and emotional maltreatment on the developing child is less recognised than the impact of other types of abuse (Brassard, 2020), despite neglect being the most ‘challenging and prevalent’ form of abuse (Hibbard, 2020).
A recent review of systems to protect children from severe disadvantage (Walsh, 2018, p. 20) found childhood abuse, neglect and other ACEs to have been associated with subsequent psychosocial disorders. These include behavioural problems, attention-deficit hyperactivity disorder diagnosis in middle childhood, bipolar disorder, childhood autobiographical memory disturbance, chronic mental health problems, eating disorders, personality disorders, post-traumatic stress disorder, psychosis, self-harm, suicide attempts and uncontrollable anger.
Associated with neglect is the impact of institutionalisation, and the risk of extreme neglectful care. Although Rutter’s longitudinal review of the ‘spectacular progress’ demonstrated by Romanian orphans adopted in the UK, van IJzendoorn et al. (2020) in their review of the findings associated with institutionalisation associated with severe neglect showed,
- Attachment difficulties: in the sample of 471 children in 11 studies, a significantly lower proportion of securely attached children (24%) was found in the institution-based children compared with the normative proportion (62%); in addition, there was a much higher rate (57%) of the two most dysregulated types of attachment (insecure-disorganised and unclassifiable) compared with the normative proportion (15%);
- Delayed physical growth, brain development, cognitive development and attention: within the institutionalised group of children at least 80% were below the mean for the comparisons;
- A dose–response association: larger developmental delays and atypical development were predicted by longer stays in the institution.
8. Spanking and adult mental health impairment: The case for the designation of spanking as an Adverse Childhood Experience
Research on the impact of spanking as a form of discipline has included recommendations of classifying spanking as a significant ACE. This is one element in a world-wide movement to get societies and governments to put a stop to corporal violence and chastisement as a form of disciplining children and to encourage ‘Positive parenting’ techniques.
Afifi et al. (2017) in a review of the literature on the associated harmful impact of spanking concluded
- Spanking is defined as “the use of physical force with the intention of causing a child to experience pain, but not injury, to correct or control behaviour” but there is no evidence io its effectiveness!!
- There are similar responses associated with spanking as those associated with physical and emotional abuse
- Longitudinal studies indicate Spanking is associated with increased odds of suicide attempts, heavy drinking use of street drug
- Spanking in childhood is associated with authoritarianism in adulthood, support for punitive public policies
The specific focus on one form of ACE, and a movement to prevent it represents an example of primary prevention of ACEs.
Conclusion
This brief review of the association between ACEs and a variety of situations in children and young people’s lives demonstrates how extensive is their potential influence. It underlines the importance of developing approaches to assessment which builds on the extended range of ACEs described by Finkelhor and colleagues, and also begins to take account of the range of protective influences which mitigate against their associated impact, and to introduce preventative and targeted approaches to mitigate their impact when identified.
References
Afifi T et al (2017) Spanking and adult mental health impairment: The case for the designation of spanking as an adverse childhood experience. Child Abuse & Neglect, 71 (2017)
Baglivio MT, Epps N et al (2014). The Prevalence of Adverse Childhood Experiences (ACE) in the Lives of Juvenile Offenders. Journal of Juvenile Justice, 3(2): 1–23.
Brassard MR, Hart SN, Glaser D, et al (2020) Psychological maltreatment: an international challenge to children’s safety and well being. Child Abuse & Neglect, 110(Pt 1): 104611.
Carbone IT et al (2021). Childhood adversity, Suicidality and Non-Suicidal Self-Injury among children and adolescents admitted to emergency departments. Ann Epidemiol: 33932570
Craiga J.M., Piquerob A.R, Farrington, D.P. Ttofic M.M., (20170 Adverse childhood experiences and life-course offending in the Cambridge study. Journal of Criminal Justice 2017 53 34 -45
Dierkhising CB et al (2013). Trauma histories among justice involved youth. European Journal of Psychotraumatology, 4: 20274
Dierkhising CB et al (2019). Developmental timing of polyvictimisation. Continuity, change and association with adverse outcomes in adolescence. Child Abuse and Neglect, 87: 40 -50
Finkelhor D, Shattuck A (2012). Improving the adverse childhood experiences study scale. American Journal of Preventative Medicine, 167, 70–75.
Flaherty, E.G., Thompson, R., Dubowitz, H., Harvey, E.M., English, D.J., Everson, M., Proctor, L.J., & Runyan, D.K. (2013) Adverse childhood experiences and child health in early adolescence. JAMA Pediatrics, 167(7), 622–629
Ford T et al (2021). Recent studies of health disorders in children and young people during the pandemic. BMJ, 372: n614.
Hibbard R, Barlow J, McMillan H, et al (2020) Clinical report: psycho- logical maltreatment. Pediatrics, 130: 372–8.
Lehman S, Breivik K et al (2020). Potentially traumatic events in foster youth, and association with DSM-5 trauma and stressor related symptoms. Child Abuse and Neglect 101: 104374.
Mars B et al (2019) Predictors of future suicide attempt among adolescents with suicidal thoughts or non-suicidal self-harm: a population-based birth cohort study Lancet Psychiatry 6 327 – 339
Thompson, R., Litrownik, A.J., Isbell, P., Everson, M.D., English, D.J., Dubowitz, H., Proctor, L.J., & Flaherty, E.G. (2012). Adverse experiences and suicidal ideation in adolescence: Exploring the link using the LONGSCAN samples. Psychology of Violence, 2(2), 211-225. doi: 10.1037/a0027107.
Turner H, Finkelhor D (2020). Strengthening the predictive power of screening for adverse childhood experiences (ACEs) in younger and older children. Child Abuse and Neglect 107: 104522/
Wood S, Ford K et al (2020). ACEs in child refugee and asylum -seeking populations 2020. Public Health Wales.
van Ijzendoorn MH, Bakermans-Kraneburg MJ, Duschinsky R, et al (2020b) Institutionalisation and deinstitutionalization of children 1: a systematic and integrative review of evidence regarding effects on development. Lancet Psychiatry, 7: 703–20.
Vizard E (2013) Practitioner Review: the victims and juvenile perpetrators of child sexual abuse – assessment and intervention. Journal of Child Psychology and Psychiatry, 54: 503–15.
Back to Contents
Twenty years of ACEs research – what have we learned?
1. Lifespan outcomes of Adverse Childhood Experiences and costs to the community
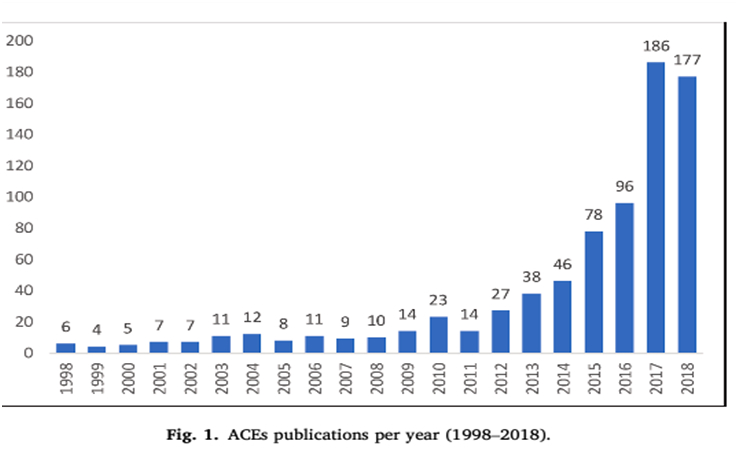
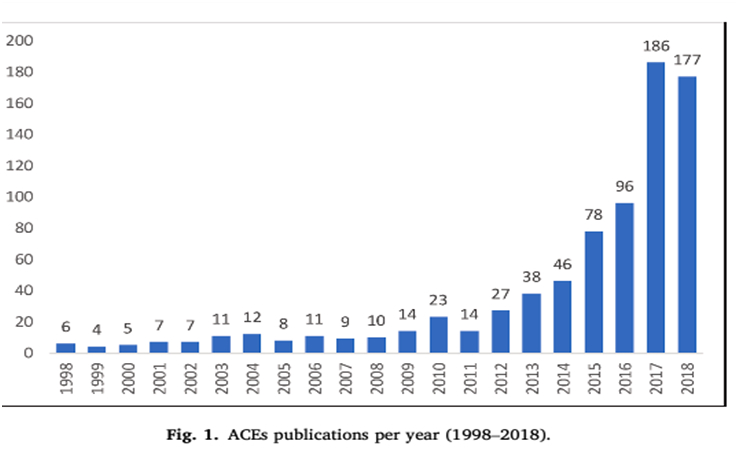
Recent papers in the January 2021 edition of the International Journal of Child Abuse and Neglect (CAN) underline the exponential growth in research in the field of ACEs in the last 20 years.
What is unique about the last 20 years research on ACEs, and how does it differentiate from the general field of child maltreatment and child protection, and what is its relevance to child and adolescent mental health?
2. Outcomes associated with ACEs
ACEs are associated with a range of poor health outcomes. For example, a meta-analysis of studies by Karen Hughes and colleagues in the Lancet Public Health (2017) of 253,719 individuals found that those individuals who had experienced at least 4 recorded ACEs reported an increased risk of poor health outcomes:
- modest – physical inactivity, overweight, obese, diabetes
- moderate – smoking, heavy alcohol use, cancer, heart disease, and respiratory disease
- strong for sexual risk taking, mental ill health, and problematic alcohol use
- strongest for problematic drug use and interpersonal and self-directed violence
- strong for sexual risk-taking, problematic alcohol use, strongest for problematic drug use, interpersonal and self -directed violence.
The associations between ACEs and mental health outcomes have been observed for ACEs examined both prospectively and retrospectively in a study at University College (Gondek, Patalay and Lacey, 2021), This was based on the Longitudinal 1958 National Child Development Study (NCDS).
Mental health-related outcomes were assessed spanning age 16-55 years. Utilisation of mental health services, taking psychotropic medications, psychological distress, life satisfaction, quality of life, and self-reported general health were measured.
- There was a robust dose-response association prospectively and retrospectively between reported ACEs and all mental health-related outcomes, regardless of whether ACEs were reported prospectively or retrospectively.
3. Costs associated with ACEs
A preliminary study of the economic costs of child maltreatment in the UK estimated that the discounted lifetime costs of non-fatal maltreatment were £89,390 per victim. Lifetime costs per death from child maltreatment were over 10 times higher, at £940,758. Bellis and colleagues (Lancet Public Health, 2019) estimated that the annual health costs associated with ACEs were US$581 billion in Europe (equivalent to 2·67% of gross domestic product) and $748 billion in north America (equivalent to 3·55% of gross domestic product).
A later study published in Lancet Public Health (Hughes et al., 2021) estimated the annual health costs linked to ACEs in 28 European countries, and found that the total ACE-attributable costs exceeded 1% of national gross domestic product (GDP) in all countries, ranging from 1·1% (Sweden and Turkey) to 6·0% (Ukraine).
These estimates were based on the associations between ACEs and health outcomes and therefore may not reflect direct costs caused by ACEs, which are nonetheless likely to be high. This research is allied to the direct costs associated with child maltreatment in the US, e.g. Fang (2012). The costs were attributed to the failures of education, mental and physical health, aggression, crime and violence associated with being subject to abuse and neglect – core adversities of childhood. The estimate was $200,000 for each maltreated individual.
4. Factors which protect against the impact of ACEs
Researchers have identified protective factors which could mitigate against poor health outcomes associated with high levels of ACEs. The Bellis Team (Bellis, 2018) described the protective value of community assets included – networking opportunities and settings to build friendships; being treated fairly; having supportive childhood friends, being given opportunities to use abilities; having a trusted adult, having someone to look up to.
Fritz and colleagues (2018) conducted a systematic review of resilience factors which moderated or mediated the relationship between childhood adversity and mental health in young people. They identified studies on individuals, the family context, and the community. Individual level protective factors which fostered resilience included mental flexibility as opposed to rigidity, a capacity to tolerate stress, high self-esteem, a secure attachment, and not ruminating on stressful events. Family factors included living in a family with a high level of togetherness, and parents who were involved with their children, and living in communities where a high level of social support was available.
Multiple resilience factors supported the development of resilience more effectively than single factors. It was concluded that resilience factors should not be studied in isolation. Interrelations between resilience factors needed to be taken into account when predicting psychopathology after childhood adversity. Resilience factors function as a ‘complex interrelated system’.
Some individuals may be genetically more or less vulnerable to stressful environmental influence and show resilience in the face of highly stressful events. This research has prompted considerable interest in ‘Protective Experiences’ (PACES) as a parallel to Adverse Experiences.
5. Strengths and limitations of the ACEs score
An ACEs profile is a cumulative risk score – reflecting challenges across multiple domains (Dube, 2021), for example, in the cycle of ACEs influencing adult mental health and functioning, influencing parenting capacities, and on the development of children and young people.
The ACEs score as a cumulative risk index has been used extensively in research studies. Lacey and Minnis (2019) in their review of 20 years research pointed out the strengths of ACEs score. It was simple to understand and carry out, and more likely to find strong, statistically significant associations with outcome, and acknowledges that adversities tend to co-occur. This observation also applies to child maltreatment research, where it has been established that forms of maltreatment co-occur, and are cumulatively associated with mental health problems (Cecil et al., 2017).
However, a limitation of the ACE score is that it assumes that each adversity has the same association with outcomes of interest – which may not be the case (e.g., sexual abuse may affect children differently to parental separation). The score in the original research was reliant on retrospective reports likely to be biased or unreliable, and many studies focus on adult outcomes rather than child outcomes. The associations between ACEs and subsequent health were correlational. Direct research is now being carried out on the adversity children experience and has begun to explore whether these associations were causal, and the pathways to poor health outcomes through prospective, longitudinal research.
Lacey and Minnis (2019) stated:
“The challenge now is to find more nuanced ways of measuring and conceptualising ACEs that are still easily usable so that detailed models of development can better inform practice and policy.”
“There is a need to carry out methodologically rigorous studies to build the evidence base of trauma-informed care as a framework and complement to trauma-specific services (p. 28).”
They advocated a variety of different approaches, e.g. studies of specific adversities – physical abuse, neglect, or sexual abuse to elucidate the mechanisms, and compare different adversities. Other approaches e.g. research on theoretically driven themes, threat, or deprivation, or person centred, latent class analysis.
A longitudinal study from University College (Bevilacqua et al., 2021) ‘explored the association between different ways of operationalising ACEs and later trajectories of internalizing, externalizing, and prosocial behavior from age 3–14’.
Three approaches to operationalising ACEs were used – ACE scores, individual ACEs, and ACEs clustering using latent class analysis. It was established in line with the general finding that a higher number of ACEs predicted worse mental health and prosocial outcomes in childhood and adolescence. In most cases these differences were evident by age 3 and persisted through to adolescence.
Exploring the impact of individual ACEs physical punishment and harsh parenting was more strongly related to externalizing behaviours, as noted in other research; parental discord and parental depression was more related to internalizing problems. In this study clustering of ACEs did not predict outcomes.
Henry et al., (2021) compared different approaches to understanding the way ACEs influence development. This included a study of Independent Risks, e.g. particular forms of adversity, the Dimensional Model of Adversity and Psychopathology (DMAP) which gathers adversities as forms of Threat and Deprivation, and the Cumulative Risk Approach.
The study demonstrated the way different models helped to understand the association of ACEs with internalising and externalising symptoms in children and young people – an important finding for the Child Mental Health field.
6. The ACEs score does not predict poor health outcomes at the individual level
An important issue is to determine whether the ACEs score being utilised in some services, and as a screening tool, can predict poor health outcomes at the individual level.
Baldwin and colleagues (2021) studied 2 birth cohorts: the Environmental Risk (E-Risk) Longitudinal Twin Study, including 2232 participants studied to aged 18 years, and the Dunedin Multidisciplinary Health and Development Study, including 1037 participants studied to age 45 years. ACEs were measured through repeated interviews and observations. ACEs were also measured retrospectively in the Dunedin study at 38 years. They reported that in line with other studies, ACE scores forecast mean group differences in health but showed poor accuracy in predicting an individual’s risk of later health problems.
They concluded:
“Targeting interventions based on ACE screening is likely to be ineffective in preventing poor health outcomes”. (E6)
Another study led by Meehan (2021) used data from the seminal ACE study (first used by Felitti et al., 1998) and found that in this ACE scores did not accurately identify individuals at high risk of health problems.
This research confirms the harmful association of ACEs with health outcomes, but demonstrates that the ACEs score does not accurately predict such outcomes at the individual level.
There is a tension between the recommendation to ascertain an ACEs score as part of an assessment of a child or young person referred to a service as a result of concerns – e.g. mental health, safeguarding, or offending services, and as a routine procedure in community services.
Gentry and Paterson (2021) carried out a rapid evidence summary of whether screening or routine enquiry for adverse childhood experiences (ACEs) meet the criteria for a screening programme.
‘Routine enquiry’: is defined where professionals ‘proactively and sensitively enquire about past childhood experiences with all service users and tailor support accordingly’
‘Screening: ‘the process of identifying healthy people who may have an increased chance of a disease or condition. The screening provider then offers information, further tests and treatment. This is to reduce associated problems or complications.’
They matched the value of ACEs screening against established criteria for screening approaches:
- The importance of the health problem being screened for – good evidence ACEs and health outcomes
- Whether cost effective primary prevention had been implemented – available but not implemented
- Whether there is a safe, precise, validated, acceptable screening test available – no consensus, suitable tool, setting, timing or frequency
- Whether there is an agreed pathway for further investigation – safeguarding for children, limited evidence for adults
- An effective intervention if given early – some evidence e.g. safeguarding, trauma-informed care
- RCT evidence for the screening programme reducing morbidity and mortality – none identified
- Whether the programme is acceptable – generally acceptable.
They concluded.
‘Routine enquiry among adults (REACH) was assessed as feasible and acceptable to service users and professionals and resulted in the delivery of potentially effective interventions…… but there was doubt whether screening or routine enquiry could improve morbidity, mortality, health and well-being (p. 7).’
7. Research on risk calculators to identify which children exposed to ACEs will develop poor health outcomes
Research which has been conducted balancing risk and protective factors to develop a risk calculator which identify which children exposed to ACEs will develop poor health outcomes. This was studied in a series of papers based on the longitudinal study of Twins in the Environmental Risk (E) study. Participants were 2232 twin children born in England and Wales in 1994–1995. Lewis et al. (2019) explored the epidemiology of trauma and post-traumatic stress. Meehan et al. (2020) studied a sub-set exposed to any type of victimisation, and Lewis et al. (2021) the impact of complex trauma.
In the subset of the E-Risk Study sample exposed to any type of victimization during childhood was studied. Victimisation included the following:
- Exposure to victimization was assessed at 5, 7, 10, and 12 years of age
- Cumulative information was gathered about exposure to domestic violence; frequent bullying by peers; physical abuse sexual abuse; emotional abuse and neglect; and physical neglect – all significant forms of adversity
- Non-complex traumas were defined as a one-off assault, an accident and learning about the sudden death of a parent.
Multivariate Risk/Resilience Predictors were established gathered from recorded experiences during the child or young person’s regular reviews:
- Individual characteristics: Sex, intelligence, personality factors, openness, conscientiousness, extraversion, agreeableness neuroticism
- Mental health was recorded during development: ADHD symptoms, conduct disorder, anxiety, depression, self-harm, psychotic symptoms
- Family and Community Factors – maternal warmth, sibling warmth, family psychopathology, socio-economic circumstances, community crime, victimisation, social cohesion, status among peers.
A psychiatric assessment was conducted when the young people were aged 18, providing detailed understanding about the associations of the associations of risk and resilience factors and mental health in early adult life, with implications for the longer term.
Psychiatric Assessment aged 18

The figure demonstrates that exposure to any trauma during childhood results in a spectrum of mental health responses measured at aged 18: Post-traumatic responses, through Depression, Anxiety, Conduct disorder, Alcohol and Cannabis dependence, Psychotic symptoms, Self-harm and Suicide attempts.
Complex trauma exposure included multiple events, interpersonal assaults or threats in childhood or adolescence, repeated child abuse, severe bullying, witnessing neighbourhood violence resulted in more extensive mental health responses.
The studies demonstrated that when the risk and resilience factors are taken into account the more risk factors and the less resilience factors the more likely the association with any Psychiatric Disorder, Internalising or Externalising disorders.
There was a risk of later complex trauma and more severe psychopathology, and cognitive deficits, when there was evidence of significant early vulnerabilities internalising and externalising symptoms at age 5 years, and family members with a history of mental illness.
A further analysis of the study (Lathem et al., 2019) demonstrated that a different set of factors were associated with risk for psychosocial disadvantage or economic disadvantage. Psychosocial disadvantage was associated with individual, family and community factors, economic disadvantage with individual and family factors. The value of being able to predict which child or young person is at risk of disadvantage is an important step to prevention. The risk calculator that was developed could be used as a reliable screening tool, with an individualised score which guides intervention.
Conclusions
This work represents an important development in the field because it demonstrates and confirms the complexity of mental health responses to exposure to trauma associated with multiple adversities. The research also established how few of the young people in the study had received treatment for traumatic responses. Considering a range of individual, family and community risk, vulnerability and resilience predictive analytic factors could better predict mental health outcomes for the individual, and guide intervention. Balancing risk factors represented in the ACEs score with resilience factors could guide the practitioner’s assessment and intervention.
8. Adverse Childhood Experiences are associated with neurobiological and inflammatory responses
The traumatic impact of various forms of maltreatment and neurobiological functioning – particularly those involving threat – physical abuse, emotional abuse and sexual abuse has been well established (Teicher et al., 2016). The association between Childhood Adversity and Abuse on later health has evoked considerable research.
A review summarising the impact of early adversity on children’s development noted that chronic stress can be toxic to the child’s development and significant early adversity can lead to lifelong problems (National Scientific Council on the Developing Child, 2008/2012). For example, when maltreatment-induced chronic elevation of cortisol occurs in the context of ‘toxic stress’, damaging effects in the brain can include deficits in memory formation and recall and impaired cognitive control over thought, emotion and behaviours, resulting in poorer later performance in school, the workplace and relationships (Vizard et al.. 2021, p. 5).
McCrory and Viding (2017) observe that neuro-biological and neuro-cognitive systems adapt to early abusive and neglectful experiences. The classical post-traumatic responses of heightened response to threat, avoidance and turning away from relationships, restricted memories provide short-term functional advantages to atypical environments, but compromise the capacity of the individual to negotiate more normative contexts or adapt to future stressor events. Latent vulnerabilities predict future psychiatric risk, before disorders emerge. Brain differences are markers of latent vulnerability at the neural level and impacts on establishing relationships in the family, school and community.
The Dunedin Multi-Disciplinary Health and Development study (Danese, 2007) investigated significant biomarkers of inflammation in adulthood, investigating links with later Inflammatory Disease. They found a significant association between childhood maltreatment in the first decade of life and elevated adult inflammatory markers such as C-Reactive Protein (CRP). It was already known that adult health outcomes linked to these inflammatory biomarkers included cardiovascular disease, diabetes and chronic lung disease. The association between childhood adversity and inflammation has since been reported in meta-analytic research (Baumeister et al., 2015) although stronger associations are found for inflammation in adulthood relative to childhood (Kuhlman et al., 2020).
Cumulative exposure to adversity may be associated with ‘allostatic overload’, beyond the usual bodily ‘wear and tear‘, and may cause the normal neurobiological responses to become pathological rather than protective, and to attack the child’s body with raised inflammatory markers. (Danese and McEwan, 2012). A link is examined between stress, cardiac responses, inflammatory responses, accelerated aging of chromosomes – telomere length and psychopathology. A variety of early adverse events – divorce, separation, physical abuse, and multiple adversity – were associated with later inflammatory responses (Nelson et al., 2021).

Lacey and colleagues (2020) based on the Longitudinal 1958 British birth cohort were able to use a variety of different models to explore the association of Adverse Childhood Experiences reported prospectively and retrospectively with inflammatory processes. Single adversities, cumulative risk and Latent Class Approaches were studied for possible associations with chronic inflammatory processes. The authors concluded that looking at combinations of ACEs could be a helpful alternative way of operationalizing ACEs.
Current research on ACEs is beginning to move from the original focus on the association with harmful outcomes with a cumulative impact of ACEs to a more nuanced understanding of the processes which underpin the longer-term impact of adversity in childhood.
Longitudinal studies looking at the later adverse impact of ACEs on children’s mental health and brain functioning suggest that early damage to a child’s developing brain is not necessarily irreversible. The brain retains plasticity throughout the lifetime and if the child has acquired sufficient life-course resilience from a relationship with an ‘always available adult’, recovery from early ACEs may be possible, at least in part (Bellis, 2017).
References
Baldwin J et al (2020). Population vs Individual prediction of poor health from results of Adverse Childhood Screening. JAMA Paediatrics, 10.1001/5602.
Baumeister, D., Akhtar, R., Pariante C.M., Mondelli, V. (2016) Childhood trauma and adulthood inflammation: a meta-analysis of peripheral C-reactive protein, interleukin-6 and tumour necrosis factor-α. Mol Psychiatry, 21, 642 – 649
Bellis MA, Hardcastle K, Ford K, et al (2017) Does continuous trusted adult support in childhood impart life-course resilience against adverse child- hood experiences – a retrospective study on adult health-harming behaviours and mental well-being. BMC Psychiatry, 17, 1, 110.
Bellis, M. A., Hughes, K., Ford, K., Rodriguez, G. M., Sethi, D., & Passmore, J. (2019). Life course health consequences and associated annual costs of adverse childhood experiences across Europe and North America; a systematic review and meta-analysis. The Lancet Public Health, 4(10), e517–528. https://doi.org/ 10.1016/S2468-2667(19)30145-8.
Bellis, M. A., Hughes, K., Ford, K., Hardcastle, K. A., Sharp, C. A., Wood, S., … Davies, A. (2018). Adverse childhood experiences and sources of childhood resilience: A retrospective study of their combined relationships with child health and educational attendance. BMC Public Health, 18, 792
Bevilaqua, L., Kelly ,Y. Heilman, A., Priest, N. Lacey, R. (2021) Adverse childhood experiences and trajectories of internalising and externalising, and prosocial behaviours from childhood to adolescence Child Abuse and Neglect 112. 104890
Cecil, C.A.M., Viding, E., Fearon, P., Glaser, D., & McCrory, E.J. (2017). Disentangling the mental health of childhood abuse and neglect. Child Abuse and Neglect, 63, 106-119.
Conti G, Morris S, Melnychuk M, et al (2017) The Economic Costs of Child Maltreatment in the UK: A Preliminary Study. NSPCC.
Danese A, Pariante CM, Caspi A, et al (2007) Childhood maltreatment predicts adult inflammation in a life-course study. Proceedings of the National Academy of Sciences of the United States of America, 104 (4): 1319-24.
Danese A, McEwan BS (2012) Adverse Childhood Experiences, allostasis, allostatic load, and age-related disease. Physiology and Behavior, 106 (1): 29-39.
Fang X, Brown D.S., Florence C.S. and Mercy ,J.A. (2012) The economic burden of child-maltreatment in the United States and implications for prevention Child Abuse and Neglect 36, 156 – 165
Fritz J., de Graaff A.M. Caisley ,H. van Harmelen, A .Wilkinson P.Q. (2018) A Systematic Review of Amenable Resilience Factors That Moderate and/or Mediate the Relationship Between Childhood Adversity and Mental Health in Young People3.frontiersin.org/articles/10.3389/fpsyt.2018.00230/full?report=reader
Gondek, D., Patalay P, Lacey R.E (2021) Adverse childhood experiences and multiple mental health outcomes through adult a prospective birth cohort study J. Public Health , https://doi.org/10.1093/pubmed/fdy0992018
Gentry, S.V. Paterson, B.A., (202), Does screening or routine enquiry for adverse childhood experiences (ACEs) meet criteria for a screening programme? A rapid evidence summary, Journal of Public Health, fdab238, https://doi.org/10.1093/pubmed/fdab238
Henry L.M., Gracey K., Shaffer A. et al (2021) Comparison of Three Models of Adverse Childhood Experiences: Associations With Child and Adolescent Internalizing and Externalizing Symptoms Journal of Abnormal Psychology 130 , 9 -2
Hughes K, Bellis MA et al (2017). The effect of multiple adverse childhood experiences on health: A systematic review and meta-analysis. The Lancet Public Health 2: 356–366.
Hughes, K., Ford, K., Bellis, M.A., Glendinning, F., Harrison, E., Passmore, J. (2021) Health and financial costs of adverse childhood experiences in 28 European countries: a systematic review and meta-analysis The Lancet – Public health, 6 e848- e857
Kuhlman, K. R., Horn, S. R., Chiang, J. J., & Bower, J. E. (2020). Early life adversity exposure and circulating markers of inflammation in children and adolescents: A systematic review and meta-analysis. Brain, Behavior, and Immunity, 86, 30-42
Lacey R & Minnis H (2019). Practitioner Review: Twenty years of research with adverse childhood experience scores – Advantages, disadvantages and applications to practice. Journal of Child Psychology and Psychiatry, 61(2), 116–130.
Lacey R. Pinto Pereira S.M, Danese A., (2020) Adverse childhood experiences and adult inflammation: -Single adversity, cumulative risk and latent class approaches. Brain, Behavior, and Immunity 87 820–830
Latham R.M., Meehan A.J., 2019 Arseneault, L, Danese A., Fisher, H.L (2019 ) Development of an individualised risk calculator for poor functioning in young people victimised in childhood: a longitudinal cohort study Child Abuse and Neglect 98 104188
Lewis, S.J., Arseneault, L, Caspi, A., Fisher, H.L., Mathews, T., Moffitt, T., & Danese, A. (2019). The epidemiology of trauma and post-traumatic stress disorder in a representative cohort of young people in England and Wales. Lancet Psychiatry, 6, 247 – 256.
Lewis S. et al (2021) Unravelling the contribution of complex trauma to psychopathology and cognitive deficits: a cohort study. BJPsych 2021 419-455
McCrory, E., Gerin, M. I., & Viding, E. (2017). Child maltreatment. Latent vulnerability, and the shift to preventative psychiatry – The contribution of functional brain imaging. Journal of Child Psychology and Psychiatry, 58, 338–357.
Meehan AJ et al (2020). Developing an individualised risk calculator for psychopathology among young people victimised during childhood: a population- representative cohort study, J Affective Disorders 262 90 -98.
Meehan A.J. , Baldwin ,J. Lewis, S.L. Macleod J.G., Danese A. (2021) Poor Individual Risk Classification from Adverse Childhood Experiences Screening Am J. Prev. Med. Doi:10.1016?jamepre.2021.08.008
National Scientific Council on the Developing Child (2008/2012) Establishing a Level Foundation for Life: Mental Health Begins in Early Childhood (Working Paper No. 6) (Updated Edition). Center on the Developing Child, Harvard University.
Nelson B.W, Sheeber L., Pfeifer J. Allen N.B 2021 psychobiological markers of allostatic load in depressed and non-depressed mothers and their adolescent offspring Journal Child Psychology & Psychiatry 62, 199 -211
Struck S, Syewart-Tufesco A et al (2021). Adverse childhood experiences (ACEs) research: A bibliometric analysis of publication trends over the first 20 years. CAN 112: 104895
Teicher, M. H., Samson, J. A., Anderson, C. M., & Ohashi, K. (2016). The effects of childhood maltreatment on brain structure, function and connectivity. Nature Reviews Neuroscience, 17, 652–666. https://doi.org/10.1038/nrn.2016.111.
Thompson, R., Litrownik, A.J., Isbell, P., Everson, M.D., English, D.J., Dubowitz, H., Proctor, L.J., & Flaherty, E.G. (2012). Adverse experiences and suicidal ideation in adolescence: Exploring the link using the LONGSCAN samples Psychology of Violence, 2(2), 211-225. doi: 10.1037/a0027107.
Vizard, E., Gray, J., & Bentovim, A. (2021). The impact of child maltreatment on the mental and physical health of child victims: A review of the evidence. BJPsych Advances, 1-11. doi:10.1192/bja.2021.10
Available from: https://www.cambridge.org/core/journals/bjpsych-advances/article/impact-of-child-maltreatment-on-the-mental-and-physical-health-of-child-victims-a-review-of-the-evidence/D5A662192092FADD5E9F594B65C083FA/share/bf4f35a8cd7c6f7fbd92ed4bf8c44e8c13b88247
Back to Contents