Abstract
Depression is common but the biological mechanisms leading to this disorder are not well understood. The link between inflammation and the brain may help us elucidate a potential mechanism. Inflammatory mediators are associated with multiple changes in the brain that can result in alteration to mood and behaviour. As such, reducing inflammation may be an effective measure to control depressive symptoms in certain individuals.
Background
Most of us will experience depressive symptoms at some point in our lives and depression diagnoses are on the rise, particularly in young people (1) (Figure 1). Despite depression being very common, it remains a relatively poorly understood disorder. In the not-so-distant past, mood disorders were rarely talked about in public or in private. We know that family history of depression, traumatic experiences, and different life events can put people at risk of depression. But what is the biological mechanism behind these associations? One possible answer lies within the immune system.
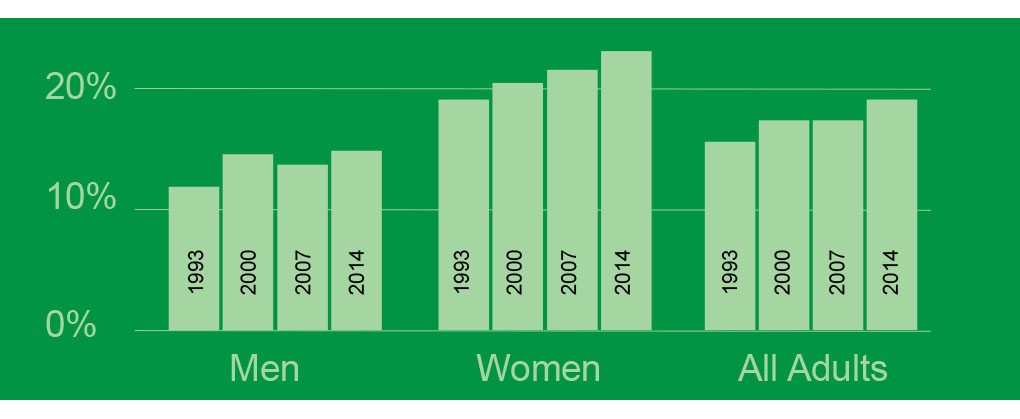
Figure 1. The percentage of the UK experiencing common mental health problems is increasing.
Research has shown that persistent low-grade inflammation (PLGI) is associated with subsequent depression (2). The link between PLGI and later depressive symptoms can be seen as early as childhood. Early life trauma, autoimmune disorders, recurrent infection, exposure to irritants, and certain lifestyle factors all increase the levels of inflammatory mediators (e.g. IL-6 and CRP) (3–5). Inflammatory mediators are messengers that act on blood vessels and/or cells to promote an inflammatory response, therefore an increase in inflammatory mediator levels also increases systematic inflammation (3–5).
Considerable evidence exists to show that inflammatory mediators induce symptoms of depression, such as low mood and concentration difficulties (6). Mood and behaviour may be altered by inflammatory mediators in a number of ways. First, PLGI can lead to a reduction in the levels of dopamine, serotonin, and noradrenaline, resulting in chemical imbalances in the brain. Inflammatory mediators may also induce glucocorticoid resistance and subsequently raise plasma levels of cortisol, the stress hormone. Inflammation also promotes excitotoxicity, excessive stimulation of nerve cells that damages/kills cells, and impairs adaptive neuroplasticity (7,8). To complicate matters, depression itself also promotes inflammatory reactions (8). Individuals with depression develop negative health behaviours such as sedentary lifestyle, poor diet, obesity, poor sleep, and smoking that can lead to uncontrolled inflammation (9). For example, poor diet may lead to obesity and important changes in microbiota composition which in turn play important roles in inflammation (8,10) (Figure 2).
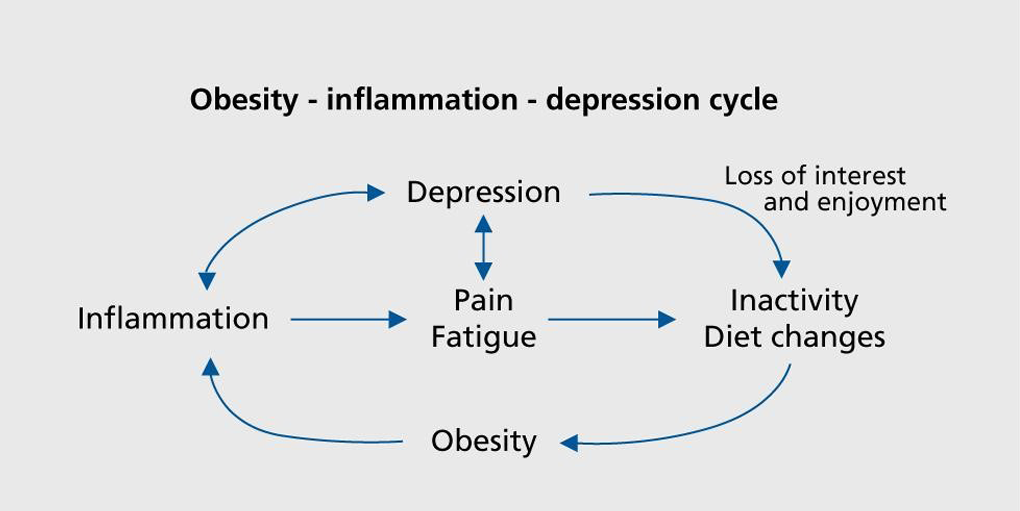
Figure 2. The relationship between inflammation and depression is bidirectional.
While it is tempting to assume that inflammation is an important risk factor for depression in all individuals, depression is a heterogenous condition and people experience symptoms differently. The number of subtypes of depression that have been described illustrates this point. Given that approximately one third of individuals with depression show evidence of PLGI, it is plausible that PLGI is associated with specific subtype(s) of depression (11). For example, PLGI shows greater association with atypical than melancholic depression (4,12). Atypical depression is generally characterised by hypersomnia, fatigue, apathy, and overeating. White adipose tissue in turn produces inflammatory mediators that contribute to pathogenic immunometabolic responses in the central nervous system, brain, and rest of body (5). Therefore, being overweight may contribute to the risk of depression via inflammatory processes (10). Interestingly, some studies have found that the Mediterranean diet may be protective against risk of depression and inflammation (13,14).
Implications
Does all this research this mean that inflammatory mediators are clinically useful for identifying individuals at risk of (atypical) depression? A similar percentage of individuals that show signs of PLGI also do not respond to anti-depressants suggesting that there may be a link between these two observations (11). High levels of inflammatory mediators may therefore be effective at identifying people with depression who are likely to need alternative treatment to anti-depressants. However, while anti-inflammatory drugs can reduce inflammation, it is unclear whether these drugs also reduce depressive symptoms. The Insight Study at Cambridge University is currently investigating the answer to this question (11).

The implications of this is that interventions to help people with depression that is not responsive to anti-depressants can be found. This means that people with different subtypes of depression can be treated with slightly more personalised medicine. However, whether PLGI can identify individuals at risk of depression is still debatable.
Conclusions
PLGI is one potential mechanism leading to higher risk of depression, particularly atypical depression. This inflammation can result from multiple life experiences including early life trauma, and maybe a viable target to reduce or prevent depressive symptoms. More research is needed to understand risk factors and biological mechanisms for depression, particularly in young people.
Conflict of interest
The author is describing research from the field within which she works, although she was not directly involved in any of the research referenced. The author has no financial interest in the work presented.
References
(1) McManus S, Bebbington P, Jenkins R, Brugha T. Mental health and wellbeing in England: Adult Psychiatric Morbidity Survey 2014. Leeds: NHS Digital. [Internet]. eds. 2016 [cited 2018 Nov 28]. Available from: https://digital.nhs.uk/data-and-information/publications/statistical/adult-psychiatric-morbidity-survey/adult-psychiatric-morbidity-survey-survey-of-mental-health-and-wellbeing-england-2014
(2) Khandaker GM, Pearson RM, Zammit S, Lewis G, Jones PB. Association of Serum Interleukin 6 and C-Reactive Protein in Childhood With Depression and Psychosis in Young Adult Life: A Population-Based Longitudinal Study. JAMA Psychiatry. 2014 Oct 1;71(10):1121–8.
(3) Pahwa R, Jialal I. Chronic Inflammation. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2019 [cited 2019 Sep 4]. Available from: http://www.ncbi.nlm.nih.gov/books/NBK493173/
(4) Penninx BWJH. Depression and cardiovascular disease: Epidemiological evidence on their linking mechanisms. Neurosci Biobehav Rev. 2017 Mar 1;74:277–86.
(5) Hohmann CF, Odebode G, Naidu L, Koban M. Early Life Stress Alters Adult Inflammatory Responses in a Mouse Model for Depression. Ann Psychiatry Ment Health [Internet]. 2017 [cited 2019 Sep 4];5(2). Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5898393/
(6) Dantzer R, O’Connor JC, Freund GG, Johnson RW, Kelley KW. From inflammation to sickness and depression: when the immune system subjugates the brain. Nat Rev Neurosci. 2008 Jan;9(1):46–56.
(7) Haroon E, Raison CL, Miller AH. Psychoneuroimmunology Meets Neuropsychopharmacology: Translational Implications of the Impact of Inflammation on Behavior. Neuropsychopharmacology. 2012 Jan;37(1):137–62.
(8) Bauer ME, Teixeira AL. Inflammation in psychiatric disorders: what comes first? Ann N Y Acad Sci. 2019;1437(1):57–67.
(9) Berk M, Williams LJ, Jacka FN, O’Neil A, Pasco JA, Moylan S, et al. So depression is an inflammatory disease, but where does the inflammation come from? BMC Med. 2013 Sep 12;11(1):200.
(10) Shelton RC, Miller AH. Inflammation in depression: is adiposity a cause? Dialogues Clin Neurosci. 2011;13(1):41–53.
(11) The Insight Study [Internet]. Welcome to Immunopsychiatry: Inflammation and Psychiatry Research Group, Cambridge. [cited 2019 Sep 4]. Available from: http://www.immunopsychiatry.com/the-insight-study.
(12) Lamers F, Milaneschi Y, Penninx BWJH. Chapter 26 – Depression Subtypes and Inflammation: Atypical Rather Than Melancholic Depression Is Linked With Immunometabolic Dysregulations. In: Baune BT, editor. Inflammation and Immunity in Depression [Internet]. Academic Press; 2018 [cited 2019 Sep 5]. p. 455–71. Available from: http://www.sciencedirect.com/science/article/pii/B978012811073700026X.
(13) Dai J, Miller AH, Bremner JD, Goldberg J, Jones L, Shallenberger L, et al. Adherence to the mediterranean diet is inversely associated with circulating interleukin-6 among middle-aged men: a twin study. Circulation. 2008 Jan 15;117(2):169–75.
(14) Willett WC, Sacks F, Trichopoulou A, Drescher G, Ferro-Luzzi A, Helsing E, et al. Mediterranean diet pyramid: a cultural model for healthy eating. Am J Clin Nutr. 1995;61(6 Suppl):1402S-1406S.