A children’s wellbeing practitioner (CWP) is a highly specialist role in a CAMHS team. CWPs deliver low-intensity psychological interventions for mild to moderate low mood and anxiety disorders. We treat children and young people using a variety of interventions such as:
- Behavioural Activation
- Graded Exposure
- Worry management
- Parent-led CBT
Initial Assessments
A psychological wellbeing practitioner (PWP) will start the therapeutic process by offering an initial assessment, in order to gather more information about the presenting problem. This is an important part of the process as it allows the PWP to develop a CWP formulation, which helps with moving onto the intervention stage (Curry, Dunsmuir & Fuggle’s, 2012).
A CWP’s initial assessment is different to a generic CAMHS clinician. It has a tight structure and a short time slot. The initial assessment can be broken down into 3 sections: information gathering, information giving and shared decision making (Reach Out).
The information gathering section of the assessment can be broken down into four key elements: 4’w’s, 5 areas formulation, impact and risk. The 4 W’s explore the presenting problems in terms of; what is the problem? where does it happen? with who is the problem better or worse and when does this happen? These four brief questions allow for the practitioner to be time efficient in this area of the assessment (Richards & Whytes, 2011). Following the 4 W’s we complete a 5 areas formulation, identify impact and complete a risk assessment.
According to the “Reach Out” document, the next steps after completing the information gathering section are to complete a problem statement, create patient-centred goals and give treatment information (Richards & Whytes, 2011). A problem statement draws a conclusion to the initial assessment. I try to encourage the young person to write their own problem statement with some verbal help from myself. Once a problem statement is completed we can then think about setting goals and the intervention we are going to use.
Typical day as a CWP
Following the initial assessment we will meet with the young person to complete a collaborative 5 areas formulation. During this session we also review the RCADS and start the joint decision-making approach to decide which intervention we are going to use.
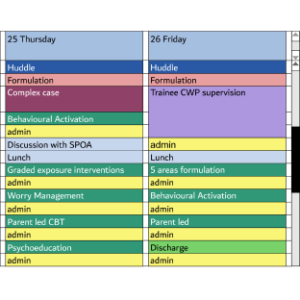
A typical day for a CWP will always include a number of 30 minute intervention slots. We usually see our patients weekly or fortnightly. Preparation is needed for these appointments as they often rely on the use of worksheets for homework/tasks. We see the young person for around 30 minutes which allows for us to provide feedback to the parents/carers. Once we have done this feedback we have a brief window to add a case note and make any other changes.
Summary of a typical intervention – BA for depression
- Treatment Session 1 (with parents): Young person and parents (1 hour). The CWP provides psycho-education about depression. We will also discuss the treatment rationale with a brief personalised exploration of the model (Homework-Activity monitoring form). We will complete RCADS.
- Treatment Session 2 (30 minutes): A review of the daily monitoring form with a treatment rationale review. During this session we will look at what activities provide positive and negative reinforcement and consider the balance of activities. (Homework is continued activity monitoring and balancing of activities).
- Treatment Session 3 (30 Minutes): A review of daily monitoring forms and activity targets. We will then complete a values-based assessment task where we look at different areas in the young person’s life such as family, friends, hobbies, self-care, future plans and physical health. We will then generate one activity to try. (Homework is to review the diary exercise and introduce one activity target).
- Treatment Session 4 (30 minutes): A review of the values-based activity task. Then, the generation of a list of activities to inform activity scheduling. We will commence activity planning and scheduling using ACE logs and activity scheduling sheets. (Homework is 3 activity targets).
- Treatment Session 5: A review of the daily monitoring form. We continue activity planning and scheduling using ACE logs and activity scheduling sheets. (Homework is 3 activity targets).
- Treatment Session 6 (with parents 1 hour: A review of progress and continued activity planning and scheduling, using ACE logs and activity scheduling sheets, with some problem solving. (Homework is to add or remove or adjust activities based on learning).
- Treatment Session 7: Continue activity planning and scheduling using ACE logs and activity scheduling sheets. Problem solving and thinking about any areas left to work on. (Homework is to add or remove or adjust activities based on learning).
- Session 8 and beyond (with parents): We complete a relapse prevention exercise. A review of learning and accomplishments. CWP will provide advice: including top tips for staying well.
- Discharge – planning for the end of treatment (with parents): Complete progress review and finalise relapse prevention plan. Complete RCADS again.
A Typical CWP’s Diary is below:
Providing supervision
Another part of our role as a qualified CWP is to provide clinical and caseload management to trainee CWPs. This supervision is weekly as trainees have a set number of hours of required supervision for their course. Supervision is to ensure that trainees have access to suitable cases and to check that they are able to stick to their evidenced-based model of treatment.
Working alongside Single Point of Access to CAMHS
As CWPs we work very closely with the Single Point of Access Team to ensure that our initial assessment are selected to be mild to moderate in risk. This ensures that chosen cases benefit from our specific structured model. A CWP model may not be appropriate if there is complexity or risk or if there are neurodevelopmental concerns that need to be assessed.
Formulation and team working
As a CWP we have weekly formulation slots in our diary. Clinicians can book a half hour slot to discuss a young person that they would like to refer to us for low intensity work. During this discussion a CWP will think about previous work undertaken, risk and complexity. A CWP will work with children and young people who need further work, after completing a tier 3 CAMHS intervention.
Once a young person has completed a low intensity intervention such as BA, the CWP can then think about other interventions that the young person may benefit from such as Graded Exposure.
If a CWP is worried about a child, and thinks they may need higher intensity work, we can discuss this with the tier 3 team through supervision, formulation or case discussion.
Attending complex case discussion
As part of working in a generic CAMHS team, a CWP will attend a weekly complex case discussion. The form of the complex case discussion depends on what the clinician who is presenting wants from the meeting. One aim may be to think about a plan/future work for the young person. A CWP can also take a case to discuss. They may discuss a case that has gone well or a case that they feel they need support with.
I think it’s important for CWPs to take cases that have gone well, to help other clinicians in the team understand the structured role of the CWP. A CWP may also contribute with ideas about how a low intensity intervention may benefit the young person under discussion.
Working with complex cases as a low intensity worker
As discussed, a CWP will work with young people with mild to moderate (current or historical) risk to do a specific piece of work to help meet the goals of the young person. The lead professional continues to hold the case and manage risk whilst the CWP offers their intervention.
- Curry, V. Dunsmuir, S. Fuggle, P. (2013). CBT with Children, Young People and Families. London: S. 63-64.
- Richards, D. Whyte, M.. (2008). Reach Out. Available: https://cedar.exeter.ac.uk/media/universityofexeter/schoolofpsychology/cedar/documents/Reach_Out_3rd_edition.pdf. Last accessed 06/03/20.



